Picture this: itchy, burning skin, random stabs of pain, and a patchy rash that seems to have a personal vendetta against your comfort. Shingles isn’t just a mild inconvenience—it can knock you sideways. When I first learned about it, it was from my nan, who swore by every home remedy under the sun. None of them worked, but she would have done anything for relief. Fast forward to today—despite antivirals being the gold standard, people still scour the internet searching for pain relief, asking if betamethasone can help. The answer isn’t quite as simple as you might hope. But let’s really get into what’s what.
What Is Shingles and Why Is It So Awful?
Shingles (doctors call it herpes zoster) is what you get when the chickenpox virus you had as a child wakes up from its lifelong nap inside your nerves. If your immune system drops its guard—thanks to stress, age, or illness—the virus reactivates, travels down nerves, and pops up as blisters and pain along one side of your body. Think of it like a surprise party from your own body, except it’s managed by a sadistic party planner.
The early signs are sneaky: tingling, burning, a brick-heavy tiredness. Within days, the rash rears its ugly head. We’re talking angry red blisters that hang out in a neat line, usually on your torso, sometimes your face. Less common but extra brutal is when shingles affect your eyes or ears. It’s not just painful—it can be downright dangerous, leading to problems like vision loss.
Pain is the main complaint. For some, it’s a burning or stabbing under the skin. Others get a constant ache that wouldn’t be out of place in a horror film. And it doesn’t always leave when the rash fades; postherpetic neuralgia—the chronic pain some feel even after the shingles rash is long gone—can last for months or even years.
The stakes get higher if you’re older. About a third of us will get shingles in our lifetime, with the risk shooting up once you pass 50. People with diabetes, cancer, or anyone with a tired immune system are on the shortlist, too. If you’re dealing with a loved one who’s had it (my mate Martin was laid up for weeks after getting shingles on his scalp), you know just how nasty this infection can be.
Betamethasone: Steroid Creams and Their Usual Role
So why are we talking about betamethasone? It’s a corticosteroid, a man-made version of hormones your adrenal glands whip up to fight inflammation fast. Doctors often use it as a cream or ointment for stuff like eczema, psoriasis, and allergic reactions. When applied, it cools the fire of inflammation, shrinking swelling and knocking out itching. In its pill or injection forms, it’s reserved for more serious inflammation inside the body—think arthritis, asthma flare-ups, or nasty allergic reactions.
Steroids like betamethasone aren’t your typical painkillers. They don’t numb the skin or zap the virus. Instead, they muffle the body’s immune response to stop the messy side effects—swelling, itchiness, and redness. That’s handy if your immune system goes overboard, but in the case of an active infection, it becomes a double-edged sword. Steroids can sometimes slow healing or even help the virus boss things around. Not exactly ideal if you want to clear up an infection, right?
When you read the leaflet that comes with a tube of betamethasone, shingles doesn’t appear on the list of things it’s approved for. Still, desperate times make people creative, which is why the internet is full of stories where people slathered on steroid creams hoping for relief.
Doctors sometimes use steroids on the skin for other blistery, itchy conditions where the immune system’s reaction is a bigger deal than any infection. With shingles, though, the story is different—and the risks can be much higher.

Can Betamethasone Help Shingles? What the Facts Say
The internet has all sorts of claims—some say betamethasone for shingles is a miracle, others warn it could make things worse. What’s the real story?
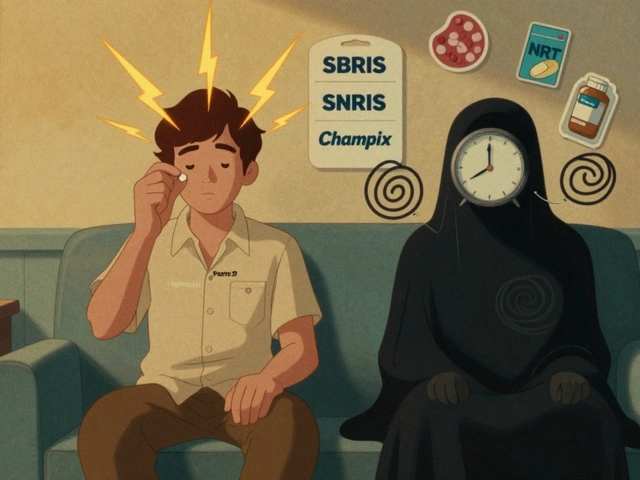
Research has looked at whether steroids, by mouth or IV, make a difference for folks with shingles. A few studies found steroids, when used alongside antivirals like acyclovir, can boost recovery speed a little and maybe cut back on short-term pain. But here’s the catch: those steroids were strong pills, not creams, and always paired with antiviral meds that actually fight the virus. No study says betamethasone alone can cure shingles, or keep away the torment of postherpetic neuralgia (that’s the nerve pain sticking around after the rash leaves).
As for cream? The virus lives deep inside nerve cells, far out of reach from anything you can rub on your skin. Steroid creams like betamethasone may temporarily ease itching at the surface, but they won’t stop the virus. Worse, putting steroids on blisters can slow your skin’s natural healing or even invite extra bacterial infections. The NHS is pretty clear: don’t use topical steroids on shingles blisters. They aren’t recommended, and you could easily get stung with new problems on top of the old ones.
Sometimes folks ask about combining betamethasone with other things, like antibiotics or antifungal creams. Again, unless your doctor finds a separate infection on your skin (which does happen, especially if the blisters get scratched open), it’s not a good idea to start mixing creams at home. Medical advice from your GP always wins out over something you read in a Facebook group.
Just last year, the British Journal of Dermatology published a roundup of all the best treatments for shingles. Antiviral tablets—acyclovir, famciclovir, valacyclovir—still rule when taken within 72 hours of the first rash. Painkillers like paracetamol, ibuprofen, or even stronger stuff can help with the agony. In cases where eye or facial nerves are involved, steroid pills given alongside antivirals might help (but this is strictly specialist territory). For everyone else, creams don’t make the cut.
Despite the horror stories about pain, using betamethasone cream for shingles just isn’t backed up by the science or guidelines. If anything, sticking to antivirals and managing pain with safer options is the way forward—your future self (and your skin) will thank you.
The Best Ways to Manage Shingles at Home—and When To See a Doctor
No one’s thrilled to have shingles, but there are tricks and tips that make the ride a bit less bumpy. First up: see your GP quickly. Antiviral tablets work best the sooner you start, ideally within three days of that first tingle or blister. If you’re over 50, immunocompromised, or the rash is on your face/eyes/ears, don’t wait. Get checked out pronto.
At home, try the following:
- Keep blisters clean and dry—this stops new infections from piling on.
- Wear loose, soft clothing. Anything that rubs or sticks will up the misery factor.
- Use cool compresses (not ice) on the blisters to take the edge off itching and swelling.
- Avoid tight bandages or anything that traps heat or dampness against the rash.
- Non-steroidal painkillers (paracetamol and ibuprofen) usually help with discomfort. Sometimes, doctors prescribe codeine or even gabapentin for severe nerve pain.
- If you’re itching to distract yourself, gentle activities like puzzles or easy walks sometimes help focus your brain elsewhere.
Definitely avoid: scratching (it spreads germs), popping blisters, or applying any steroid creams unless your doctor has checked you out in person and said it’s safe—rare, but sometimes possible under medical supervision for especially nasty itch, never on open blisters.
When should you head to the doctor right away? If your rash spreads to your eyes, gets super red or pus-filled (sign of a secondary infection), or you can’t control your pain—even with normal tablets. Kids, older adults, and folks with diabetes or immune system problems need closer monitoring. For kids like Jeremy, vaccines are the magic shield—though here in the UK, shingles vaccines are mostly offered to older adults.
The wildest fact I learned writing this? Even after a shingles attack clears up, some people keep mild aching or tingling on the same patch of skin for months or years. It’s not common, but it’s a good reason to get help early and not to soldier on alone.
The bottom line: while betamethasone has its place for many skin conditions, shingles isn’t one of them—at least, not as a cure or primary treatment. Get the right meds on board, take care of your skin, and talk to your GP before trying anything new. Don’t let guesswork guide you when it comes to something as cruel as shingles.




Write a comment
Your email address will be restricted to us