Probiotic Safety Checker
This tool helps you determine if a probiotic is safe for you based on your medical condition. Probiotics can be dangerous for immunosuppressed patients. Always consult with your doctor before taking any probiotics.
Enter your information above to see if your probiotic is safe.
Probiotics aren’t always safe when your immune system is turned down
Most people think of probiotics as harmless good bacteria that help with digestion. And for healthy folks, they often are. But if you’re taking immunosuppressants - whether after a transplant, for autoimmune disease, or during cancer treatment - those same probiotics can turn dangerous. It’s not a myth. It’s not speculation. It’s documented in hospitals and medical journals. People on these drugs have gotten life-threatening infections from probiotics they thought were safe.
The problem isn’t the probiotics themselves. It’s your body’s ability to fight back. Immunosuppressants like cyclosporine, tacrolimus, or prednisone don’t just calm down overactive immune responses. They weaken your entire defense system. That means even normally harmless microbes - like Lactobacillus or Saccharomyces boulardii - can slip through your gut lining, enter your bloodstream, and cause sepsis, heart infections, or fungemia. In some cases, it’s fatal.
Who’s at the highest risk?
Not everyone on immunosuppressants faces the same danger. Risk depends on how weak your immune system is, what drugs you’re taking, and what kind of probiotic you’re using.
The highest risk group? People with neutropenia - meaning their white blood cell count is below 500 cells/µL. This happens often during chemotherapy or after bone marrow transplants. In this group, the chance of developing a probiotic-related bloodstream infection jumps dramatically. One study found a 4.2-fold increase in bacteremia among bone marrow transplant patients using probiotics compared to those who didn’t.
Another high-risk group: recent organ transplant recipients - especially within the first three months. Your body is still adjusting to the new organ, and your immune system is being pushed to its limit. Even a small breach from a probiotic strain can lead to serious complications. A 2019 study in JAMA Internal Medicine showed Saccharomyces boulardii - a yeast often found in probiotics - increased the risk of catheter-related bloodstream infections by 27% in patients with central lines.
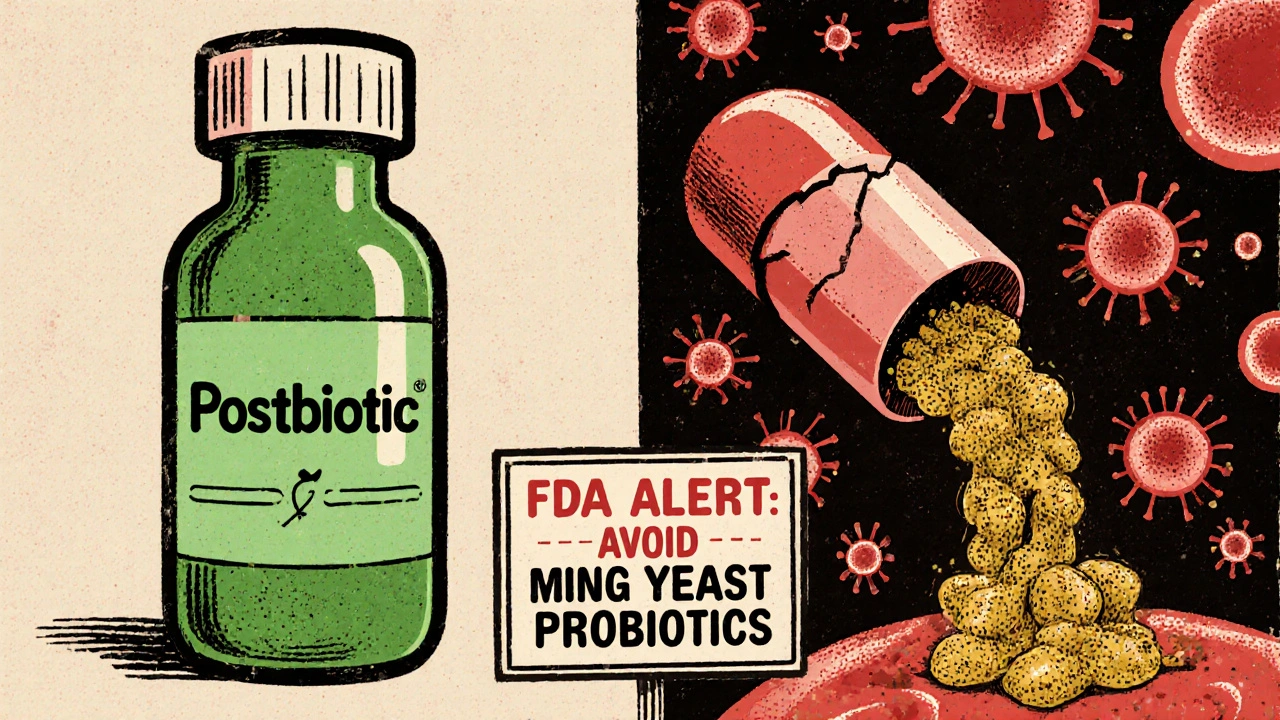
Then there’s Saccharomyces boulardii. This one’s especially dangerous. Unlike bacterial probiotics, it’s a fungus. And fungi don’t respond to regular antibiotics. When it gets into the blood of an immunosuppressed person, it can cause fungemia. Case reports show a 22% fatality rate when this happens. The FDA issued a safety alert in July 2023 specifically warning against its use in immunocompromised patients.
On the flip side, people with stable autoimmune conditions on a single drug - like methotrexate or sulfasalazine - and with decent immune function (CD4 count above 200 for HIV patients) face much lower risk. But even then, caution is needed.
What probiotic strains are safest - and which ones to avoid?
Not all probiotics are created equal. Some strains have been studied more than others. And some have clear safety profiles in immunosuppressed patients.
Strains to avoid:
- Saccharomyces boulardii - the most dangerous. Linked to multiple cases of fungemia and death.
- Multi-strain products - combinations of Lactobacillus, Bifidobacterium, and others. More strains mean more chances for something to cross the gut barrier. One 2022 study found single-strain probiotics had 63% lower translocation risk.
- Unspecified or over-the-counter blends - many don’t even list the exact strain. Without knowing the strain, you can’t assess safety.
Strains with more evidence of safety (in low-risk groups only):
- Lactobacillus rhamnosus GG - widely studied, used in some hospital protocols for diarrhea prevention. But even this strain has caused bacteremia in immunosuppressed patients.
- Bifidobacterium infantis - appears to have lower translocation potential in some studies.
- Lactobacillus plantarum 299v - approved in Europe for IBS, with limited reports of adverse events in stable patients.
The key? Always know the exact strain. Don’t buy a product labeled just “probiotic blend.” Look for the full scientific name: Lactobacillus rhamnosus GG ATCC 53103, not just “Lactobacillus.”
When might probiotics actually help?
It’s not all bad news. In some cases, probiotics can reduce infection risk - but only under strict conditions.
One of the strongest benefits is in liver transplant recipients. A 2022 meta-analysis showed probiotics reduced bacterial infections by 34% without increasing serious side effects. That’s significant. But the patients in that study were on stable immunosuppression, not in the early post-op phase.
Some hospitals use specific probiotics to prevent C. difficile infections in patients on antibiotics. But again, only in carefully selected cases. The European Society for Clinical Nutrition and Metabolism (ESPEN) still advises against probiotics in critically ill immunocompromised patients.
And now, there’s a new frontier: postbiotics. These aren’t live bacteria. They’re the harmless byproducts - like short-chain fatty acids or cell fragments - that probiotics produce. Early trials show postbiotics can reduce infections like C. difficile without the risk of bloodstream invasion. A phase 2 trial in 2024 found a 40% reduction in infection rates with no adverse events. This might be the future for immunosuppressed patients.
What do doctors actually recommend?
There’s no universal rule. But most major guidelines agree on a tiered approach.
The Infectious Diseases Society of America (IDSA) 2023 guidance breaks it down into four categories:
- Category 1 - Highest risk: Neutropenia <500 cells/µL, recent stem cell transplant, central venous catheter. Absolute contraindication. No probiotics.
- Category 2 - Moderate risk: Solid organ transplant within 3 months, severe autoimmune disease on multiple drugs. Only use after infectious disease consultation. Single-strain only.
- Category 3 - Lower risk: Stable autoimmune disease on one drug, CD4 >200. Selective strains only. Monitor for fever or GI changes.
- Category 4 - Low risk: No immunosuppression. Standard probiotic use is fine.
Many hospitals now have formal protocols. In 2023, 62% of U.S. academic medical centers had written guidelines for probiotic use in immunosuppressed patients - up from 28% in 2018.
And here’s something most patients don’t realize: if you’re on immunosuppressants and your doctor says it’s okay to take probiotics, they should be documenting the exact strain, dose, and reason. If they’re not, ask why.
What should you do if you’re on immunosuppressants?
Here’s a simple checklist:
- Don’t start any probiotic without talking to your doctor. Even if it’s “natural.”
- Stop immediately if you develop fever over 38.3°C (101°F), chills, or new abdominal pain. These could be signs of infection.
- Check the label. Is the strain listed? Is it Saccharomyces boulardii? If not, ask your pharmacist or doctor.
- Avoid probiotics during active chemotherapy or neutropenia. 87% of U.S. cancer centers advise this.
- Don’t rely on Reddit or Instagram advice. Personal stories aren’t medical evidence. One person’s “it worked for me” doesn’t override clinical risk.
And if you’re considering probiotics for digestive issues - which many autoimmune patients do - talk to your doctor about alternatives. Prebiotics (fiber that feeds good bacteria), dietary changes, or even postbiotics may be safer options.
The bottom line
Probiotics are not a one-size-fits-all supplement. For healthy people, they can help. For people on immunosuppressants, they can kill.
The data is clear: the risks are real, the consequences can be deadly, and the guidelines are evolving. What worked for your cousin after antibiotics won’t be safe for you after a kidney transplant. And just because a product is sold in a health food store doesn’t mean it’s safe for your condition.
If you’re on immunosuppressants, your immune system is already playing defense with one hand tied behind its back. Don’t let a probiotic bottle be the thing that slips through the cracks.
Can I take probiotics if I’m on prednisone?
It depends. If you’re on low-dose prednisone for a stable condition like rheumatoid arthritis, and your immune system isn’t severely suppressed, some doctors may allow specific single-strain probiotics like Lactobacillus plantarum 299v. But if you’re on high doses, have other immunosuppressants, or have recent infections, avoid them. Always check with your doctor - never assume it’s safe.
Is Saccharomyces boulardii ever safe for immunosuppressed patients?
No. Saccharomyces boulardii is a yeast, not a bacterium, and it carries a much higher risk of causing fungemia in people with weakened immune systems. The FDA issued a safety warning in July 2023 specifically for this strain. It’s been linked to bloodstream infections and deaths, especially in patients with central lines or after transplants. Avoid all products containing it if you’re immunosuppressed.
Why do some doctors say probiotics are okay while others say not to take them?
It comes down to patient risk level. Some doctors see benefit in liver transplant patients or those with chronic diarrhea. Others see too much risk in any immunosuppressed person. The evidence is mixed because most studies are small. But the trend is clear: high-risk patients (neutropenia, recent transplant, central lines) should avoid probiotics entirely. For lower-risk groups, it’s a careful, individualized decision - not a blanket yes or no.
What’s the difference between probiotics and postbiotics?
Probiotics are live microorganisms. Postbiotics are the non-living byproducts they produce - like enzymes, acids, or cell fragments. Postbiotics can support gut health and reduce infections without the risk of entering the bloodstream. Early trials show promise for immunosuppressed patients, and they’re being studied as a safer alternative. You won’t find them on most store shelves yet, but they’re coming.
Are probiotics regulated like drugs?
No. In the U.S., most probiotics are sold as dietary supplements, which means they don’t need FDA approval before being sold. Companies don’t have to prove they’re safe for immunosuppressed people. The European Food Safety Authority has rejected 95% of health claims for probiotics due to lack of evidence. That means what’s on the label isn’t always reliable. Always talk to your doctor before using them.
What should I do if I already took a probiotic and I’m on immunosuppressants?
Stop taking it immediately. If you feel fine - no fever, no chills, no new stomach pain - you’re likely okay. But monitor yourself closely for the next 7-10 days. If you develop a fever over 38.3°C (101°F), nausea, vomiting, or unexplained fatigue, go to the emergency room and tell them you took a probiotic while on immunosuppressants. Early detection saves lives.








Write a comment
Your email address will be restricted to us