Ever feel wiped out after a sniffle or wonder why your allergy meds don’t lift that heavy feeling? There’s a growing body of evidence that allergies can play a major role in chronic fatigue. Understanding how the two interact can help you break the cycle, improve daily energy, and avoid endless doctor visits.
What Exactly Are Allergies?
Allergies are an immune system over‑reaction to usually harmless substances such as pollen, dust mites, foods, or chemicals. When exposed, the body releases histamine and other mediators, triggering symptoms like sneezing, itching, and swelling.
Defining Chronic Fatigue Syndrome (CFS)
Chronic Fatigue Syndrome (also called Myalgic Encephalomyelitis) is a complex disorder marked by extreme, unexplained tiredness that doesn’t improve with rest. Diagnosis rests on persistent fatigue for six months or more, accompanied by cognitive problems, unrefreshing sleep, and often worsening after physical or mental exertion.
How the Immune System Links the Two
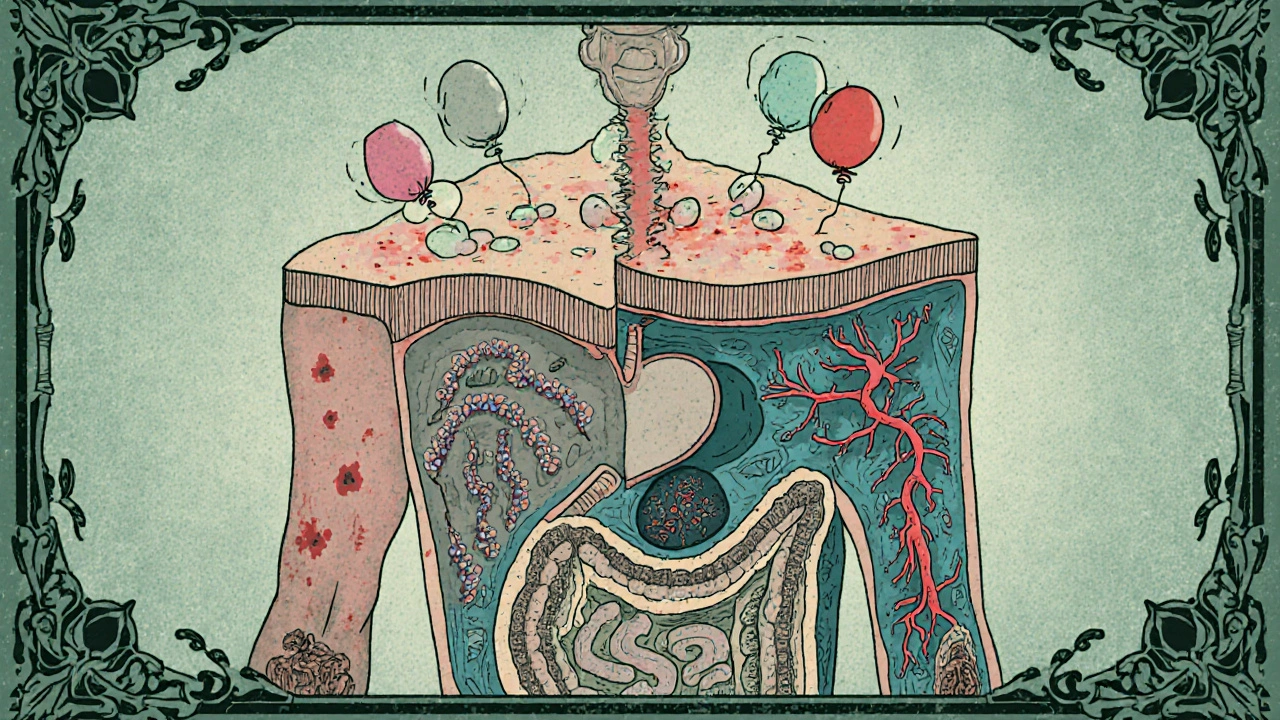
The Immune System acts as the body’s defense network. In allergy sufferers, it stays on high alert, constantly producing antibodies (IgE) and releasing chemicals. This chronic activation can lead to low‑grade inflammation, a known driver of fatigue.
Key Biological Players
Several molecules and cells sit at the crossroads of allergic reactions and energy loss:
- Histamine not only causes classic allergy symptoms but also influences sleep cycles and neurotransmitter balance, which can make you feel groggy.
- Mast Cells store and release histamine and other inflammatory mediators. Excessive mast‑cell activation has been linked to both allergic flare‑ups and chronic pain‑fatigue syndromes.
- Inflammation produced by cytokines like IL‑6 and TNF‑α can disrupt mitochondrial function, reducing cellular energy output.
Gut Microbiome: The Hidden Bridge
Research shows a disturbed Gut Microbiome can worsen both allergic responses and fatigue. An imbalance may increase intestinal permeability, allowing allergens to enter the bloodstream and keep the immune system in “defence mode.”
Hormonal Imbalance and Sleep Disorders
Allergy‑driven inflammation can affect the hypothalamic‑pituitary‑adrenal (HPA) axis, throwing off cortisol rhythms. Erratic cortisol can make you feel exhausted even after a full night’s rest. Moreover, nasal congestion often leads to poor sleep quality, which compounds fatigue.
Practical Checklist: Spotting Allergy‑Related Fatigue
- Fatigue spikes after exposure to known allergens (e.g., pollen season, pet dander).
- Morning stiffness or brain fog improves slightly after antihistamine use.
- Accompanying symptoms: sneezing, itchy eyes, skin rashes, or sinus pressure.
- Sleep appears fragmented, often due to nasal blockage.
- Blood tests show elevated IgE or eosinophil counts.
When to Seek Professional Help
If you tick more than three items on the checklist and fatigue lasts longer than three months, it’s time to consult a healthcare professional. Look for clinicians who specialize in immunology, allergy, or functional medicine. They can perform skin‑prick tests, specific IgE panels, and, if needed, refer you for a CFS assessment.

Management Strategies
- Avoid Triggers: Use HEPA filters, keep windows closed during high pollen days, and consider hypoallergenic bedding.
- Medication: Antihistamines (second‑generation) can reduce histamine‑related fatigue. For severe cases, a short course of oral corticosteroids may reset immune over‑activity, but only under doctor supervision.
- Nutrition: Support gut health with probiotics, fermented foods, and a high‑fiber diet. Vitamin D and B‑complex supplements are often depleted in chronic fatigue patients.
- Sleep Hygiene: Elevate the head of the bed, use saline nasal rinses, and practice a consistent bedtime routine.
- Stress Management: Mind‑body techniques such as gentle yoga, meditation, or paced breathing can calm the HPA axis.
Comparison Table: Allergy‑Driven vs. Non‑Allergy Fatigue Triggers
| Aspect | Allergy‑Related Fatigue | Other Common Fatigue Causes |
|---|---|---|
| Primary Trigger | Environmental allergens, foods, chemicals | Physical over‑exertion, poor sleep, anemia |
| Accompanying Symptoms | Sneezing, itchy eyes, nasal congestion, skin rash | Muscle soreness, appetite loss, weight change |
| Lab Indicators | Elevated IgE, eosinophils, cytokine spikes | Low ferritin, elevated cortisol, thyroid imbalance |
| Response to Antihistamines | Often noticeable improvement | Little to no effect |
| Seasonality | Symptoms may flare in spring/fall pollen seasons | Typically constant, unless lifestyle changes |
Frequently Asked Questions
Can allergy medication really reduce chronic fatigue?
Second‑generation antihistamines can lower histamine levels, which often eases both allergy symptoms and the associated brain‑fog. However, they work best when the fatigue is directly linked to an active allergic response.
Is mast‑cell activation syndrome (MCAS) the same as allergies?
MCAS is a more severe, systemic form of mast‑cell over‑activity. While classic allergies involve IgE antibodies, MCAS may trigger symptoms without a clear allergen, but the fatigue mechanisms overlap.
Should I get tested for food allergies if I’m constantly tired?
If you notice fatigue after meals, especially with gastrointestinal upset, a comprehensive IgG/IgE food panel can uncover hidden triggers. Elimination diets are a practical follow‑up.
How long does it take to see improvement after managing allergens?
Most people notice a reduction in fog and better sleep within 2‑4 weeks of consistent allergen avoidance and antihistamine use. Full energy recovery can take longer if chronic inflammation has built up.
Is chronic fatigue always linked to an underlying medical condition?
Not always. Lifestyle factors, stress, and sleep hygiene can cause persistent tiredness. Yet, when fatigue co‑exists with allergic symptoms, an immune‑driven cause is plausible and worth investigating.
Bottom Line
If you’ve been battling unrelenting tiredness, don’t overlook the role of allergies. Identifying triggers, getting the right tests, and combining medication with lifestyle tweaks can lift both the sneezes and the fatigue. The sooner you address the immune connection, the faster you’ll reclaim your energy and enjoy everyday life again.





Write a comment
Your email address will be restricted to us