If you have allergies and keep getting sinus infections, you’re not alone. About 30-40% of chronic sinusitis cases in the U.S. are tied to allergic reactions. It’s not just a stuffy nose - it’s constant pressure behind your eyes, thick mucus that won’t drain, headaches that won’t quit, and fatigue that lingers even after a full night’s sleep. Standard cold remedies often fail because the root cause isn’t a virus - it’s your immune system overreacting to pollen, dust, or mold. Treating this properly means going beyond antibiotics and decongestants. You need to break the cycle between allergies and sinus inflammation - and knowing when to call an ear, nose, and throat (ENT) specialist can change everything.
Why Allergies Make Sinusitis Worse
Allergies and sinusitis don’t just happen together - they feed each other. When you breathe in an allergen like ragweed or pet dander, your body releases histamine. That triggers swelling in your nasal passages and sinuses. The lining swells, mucus thickens, and tiny hair-like structures called cilia stop moving properly. That mucus gets trapped. Bacteria grow. Infection follows. And because your allergies never truly go away, the inflammation keeps coming back. This isn’t a one-time bug. It’s a cycle: allergies cause swelling → swelling blocks sinuses → blocked sinuses trap infection → infection causes more swelling → and the loop repeats. Studies show that people with allergic rhinitis are 65-75% more likely to develop chronic sinusitis than those without allergies. And once you’re stuck in this cycle, over-the-counter antihistamines alone won’t cut it. They help with sneezing and runny nose, but they don’t reduce the deep inflammation in your sinuses.First-Line Treatments That Actually Work
The most effective starting point isn’t antibiotics - it’s nasal corticosteroids. These aren’t the same as the steroids athletes abuse. These are local sprays that calm inflammation right where it’s happening. Brands like fluticasone (Flonase), mometasone (Nasonex), and budesonide (Rhinocort) are prescribed daily, one spray per nostril. They take time - 2 to 4 weeks of consistent use before you feel real relief. But once they kick in, they reduce symptoms by 65%, according to clinical trials. That’s far better than oral antihistamines like cetirizine, which only help about 42% of the time. Alongside sprays, saline nasal irrigation is critical. Using a neti pot or squeeze bottle with distilled or boiled water and a saline packet clears out allergens, mucus, and bacteria. Do it once or twice a day. But here’s the catch: if you use tap water, you risk a rare but deadly brain infection from Naegleria fowleri. The CDC has documented cases from improper use. Always use sterile water. It’s cheap. It’s simple. And it works.When Antibiotics Help - and When They Don’t
Antibiotics are often overprescribed for sinusitis. In fact, the Infectious Diseases Society of America says you shouldn’t use them for acute sinusitis unless symptoms last longer than 10 days or get worse after improving. That’s because most cases are viral or allergy-driven. But if your mucus turns thick and green, you have a fever, or your face is swollen, a bacterial infection may be setting in. In those cases, amoxicillin is still the go-to. A typical dose is 500mg three times a day for 5 to 10 days. But here’s the twist: in people with allergies, antibiotics only work about 35-45% of the time. Why? Because the inflammation is still there. The mucus is still trapped. The environment for bacteria hasn’t changed. Antibiotics kill germs, but they don’t fix the underlying blockage. That’s why treating the allergy is non-negotiable.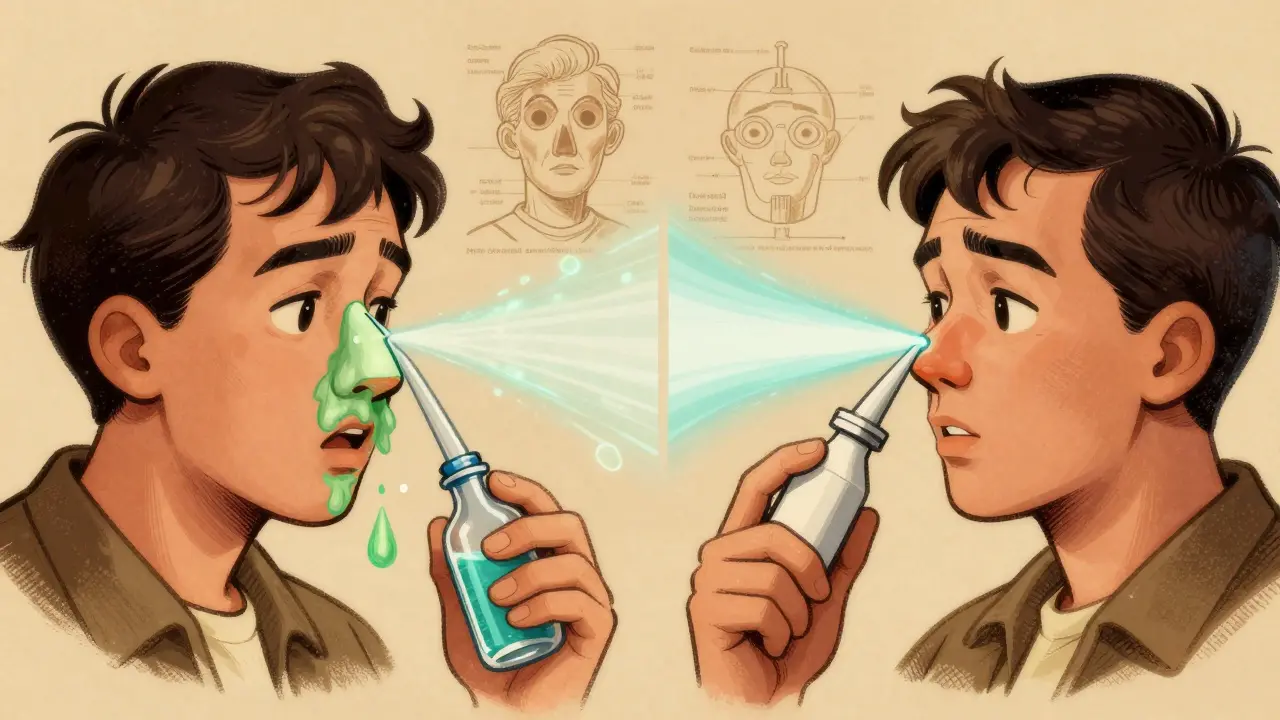
Advanced Options: Immunotherapy and Biologics
If you’re stuck in a loop of monthly sinus infections, it’s time to think bigger. Allergy immunotherapy - commonly called allergy shots - can retrain your immune system. You get weekly injections for 4 to 6 months, then monthly shots for 3 to 5 years. The payoff? 60-70% reduction in sinusitis flare-ups long-term. That’s far better than just taking meds every day. For severe cases with nasal polyps, biologics are changing lives. Dupilumab (Dupixent) blocks specific immune signals that cause inflammation. It’s given as a shot every two weeks. In trials, it reduced polyp size by 73%. Omalizumab (Xolair) and mepolizumab (Nucala) are other options, especially for people with asthma or chronic hives too. But they’re expensive - around $3,500 per month without insurance. Many insurers require proof that you’ve tried at least two corticosteroid sprays and saline irrigation first.When to See an ENT Specialist
You don’t need to wait until you’re in agony. If you’ve been on nasal steroids and saline irrigation for 4 to 6 weeks and still feel pressure, congestion, or smell loss, it’s time to see an ENT. Other red flags:- Nasal polyps - visible or confirmed by endoscopy
- Four or more sinus infections a year
- Symptoms that don’t improve after antibiotics
- Swelling around your eyes, vision changes, or severe headaches
- History of asthma or aspirin sensitivity - these often go with a condition called AERD
The Hidden Triggers You Might Be Missing
Many people focus on pollen, but indoor allergens are just as dangerous. Dust mites in bedding, mold in bathrooms, pet dander on carpets - these are constant triggers. Cleaning your home helps, but you need targeted steps:- Use allergen-proof pillow and mattress covers
- Keep indoor humidity below 50% to stop mold and dust mites
- Run a HEPA air filter in your bedroom
- Wash bedding in hot water weekly
- If you have pets, keep them out of the bedroom
New Developments on the Horizon
In 2023, the FDA approved tezepelumab (Tezspire) for severe chronic sinusitis with nasal polyps. Early results show a 56% drop in flare-ups. Researchers are also exploring microbiome therapies - using good bacteria to crowd out harmful ones in the sinuses. Early trials suggest this could cut antibiotic-resistant cases by nearly half in the next five years. Another emerging idea is intranasal antifungals for people living in damp climates. A 2024 guideline now supports their use in mold-prone areas, with patients showing 32% less symptom severity after 12 weeks.What You Can Do Today
Start simple. Buy a saline rinse kit. Get a prescription for a nasal corticosteroid. Use them every day, even if you feel fine. Track your symptoms in a journal: when you feel blocked, what you were exposed to, what helped. If after six weeks you’re still struggling, book an ENT appointment. Don’t wait for another infection. Don’t assume it’s just "allergies." Chronic sinusitis in allergy sufferers is a medical condition that needs a targeted plan - not just a bottle of decongestant.Frequently Asked Questions
Can allergies cause chronic sinusitis even if I don’t have a runny nose?
Yes. Many people with allergy-related sinusitis don’t have classic sneezing or watery eyes. Instead, they feel pressure in their forehead, dull headaches, post-nasal drip, or a constant need to clear their throat. The inflammation happens deep in the sinuses, where you can’t see it. If you have recurring sinus pain, fatigue, or smell loss - even without a runny nose - allergies could still be the cause.
Is it safe to use a neti pot every day?
Yes, if you use the right water. Always use distilled, sterile, or previously boiled (and cooled) water. Tap water can contain tiny organisms like Naegleria fowleri, which can cause a rare but deadly brain infection. The CDC has recorded cases from improper use. Rinse once or twice daily is fine - just never skip the water safety step.
Why don’t antihistamines help my sinus pressure?
Antihistamines target histamine, which causes sneezing and itching. But sinus pressure comes from swelling in the sinus lining - caused by other immune signals, like cytokines. Nasal corticosteroids block those signals directly. That’s why sprays work better than pills for congestion and pressure. Antihistamines might help your eyes or nose drip, but they won’t clear your sinuses.
How long do I need to take nasal steroids before I see results?
It takes 2 to 4 weeks of daily use to reach full effect. Most people stop too soon because they don’t feel better right away. But if you use it consistently, you’ll notice less pressure, better sleep, and fewer infections over time. Think of it like building muscle - the benefit grows with time.
Are biologics worth the cost?
For some, yes. If you’ve had multiple surgeries, rely on antibiotics every few months, or can’t work or sleep because of sinus pressure, biologics can be life-changing. Dupilumab reduces flare-ups by over 70% in clinical trials. The cost is high - around $3,500 a month - but most insurance covers it after you’ve tried other treatments. Talk to your doctor about prior authorization and patient assistance programs. For people with severe disease, the quality-of-life improvement often outweighs the price.
Can children outgrow allergy-related sinusitis?
Some do, but many don’t. Children with allergic rhinitis are more likely to develop chronic sinusitis than those without allergies. Early treatment - including saline rinses, environmental controls, and sometimes immunotherapy - can reduce long-term risk. Waiting for them to "outgrow it" can lead to missed school, sleep problems, and repeated antibiotic courses. If a child has frequent sinus infections after age 5, allergy testing is recommended.







Write a comment
Your email address will be restricted to us