More than 1 in 25 pregnant women in the U.S. are now prescribed gabapentin or pregabalin - medications originally meant for seizures and nerve pain. That’s up from less than 1 in 500 just 20 years ago. But as use has surged, so have questions: Is it safe for the baby? The answer isn’t simple. It’s not a clear yes or no. It’s about weighing real, measurable risks against the very real suffering of the mother.
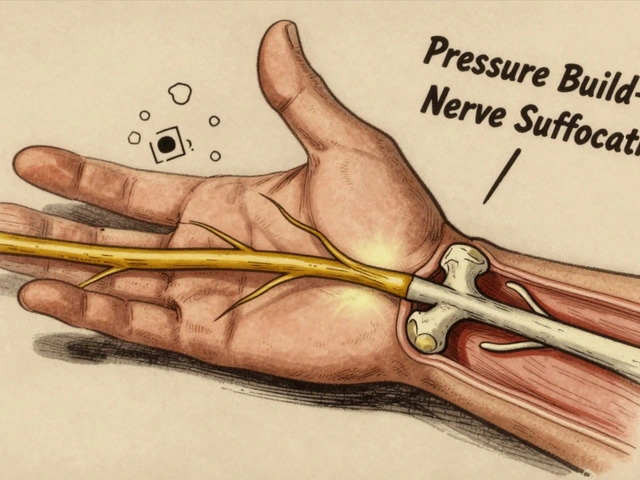
What Gabapentinoids Actually Do in the Body
Gabapentin and pregabalin are not your typical painkillers. They don’t work like ibuprofen or opioids. Instead, they calm overactive nerves by mimicking GABA, a natural calming chemical in the brain. That’s why they help with nerve pain from shingles, fibromyalgia, or even severe anxiety. But here’s the catch: they cross the placenta. Studies show they reach the baby’s bloodstream and even their developing brain tissue. Their small size and water-soluble nature make this easy. If a mom takes 300 mg three times a day, the baby is getting a steady dose too.
This isn’t just theoretical. A 2022 study using fetal tissue models found that gabapentin at therapeutic levels changed how nerve cells grow - shortening connections by up to 42%. It also turned down key genes like Nurr1 and Bdnf, which are essential for brain development. These aren’t lab curiosities. They’re signals that something biological is happening.
Birth Defects: The Big Picture
Let’s start with the most feared outcome: major birth defects. The largest study to date, tracking over 1.7 million pregnancies, found no strong link between gabapentin and overall birth defects. The risk increase? Just 0.7% - from a baseline of 3% to about 3.7%. That’s far lower than older epilepsy drugs like valproic acid, which can raise the risk to over 10%.
But one specific type of defect stood out: heart problems. Babies exposed to gabapentin, especially if the mom took it regularly during the first trimester, had a 40% higher chance of conotruncal heart defects - a group of serious conditions affecting the outflow tracts of the heart. That sounds scary, but the absolute risk is still small: 0.82% vs. 0.59% in unexposed babies. Still, when you’re talking about a baby’s heart, even small increases matter.
Preterm Birth and Growth Issues
The data gets more concerning when you look past birth defects. Babies exposed to gabapentin late in pregnancy are more likely to be born early - about 34% higher risk. They’re also more likely to be small for their gestational age. And here’s the kicker: those babies are far more likely to end up in the NICU.
One study found that 38% of babies exposed to gabapentin until delivery needed NICU care. That’s compared to just 3% of babies whose moms didn’t take it. Why? These infants often show signs of withdrawal: jitteriness, trouble feeding, excessive crying, and breathing issues. It’s not full-blown neonatal abstinence syndrome like with opioids, but it’s enough to require extra monitoring and sometimes days in the hospital.

What the Experts Are Saying
Regulators are shifting their stance. The European Medicines Agency says pregabalin should be avoided in pregnancy unless there’s no other option. The British National Formulary now calls gabapentin use in pregnancy something that needs “special consideration.” The FDA still labels both drugs as Category C - meaning animal studies showed harm, but human data is limited. In practice, that means doctors are being told: proceed with caution.
Dr. Lori Altshuler from UCLA puts it bluntly: "The overall risk of major defects is low, but the cardiac signal is real. And the NICU admission risk? That’s not negligible." She and others argue that if a woman has severe, uncontrolled neuropathic pain - pain that keeps her from sleeping, working, or caring for herself - gabapentin might still be the best option. But it shouldn’t be the first option.
When Is It Justified?
There’s no blanket rule. But here’s what most guidelines agree on:
- Don’t start gabapentin during pregnancy unless absolutely necessary.
- If a woman is already on it and doing well, don’t abruptly stop - that can trigger seizures or rebound pain.
- Use the lowest effective dose. Higher doses mean higher risks.
- Avoid use in the third trimester if possible. That’s when NICU risks spike.
- Offer fetal echocardiography if gabapentin is used consistently after week 12.
Many doctors now try alternatives first: physical therapy, acupuncture, cognitive behavioral therapy, or safer medications like duloxetine. For some women, those work. For others, they don’t. And that’s where the hard choices begin.

What About Pregabalin?
Pregabalin is often seen as the stronger, faster-acting cousin of gabapentin. But the safety data is even more concerning. Animal studies show clearer signs of developmental harm. While human data is still limited, early signals suggest it may carry a higher risk of birth defects and NICU admissions than gabapentin. That’s why experts are already seeing a drop in its use during pregnancy - and why regulators are pushing for stricter limits.
The Bigger Picture: Why Are So Many Women Prescribed This?
Gabapentin prescriptions in pregnant women jumped nearly 20-fold between 2000 and 2014. Why? Partly because it was seen as a safer alternative to opioids. But also because it was prescribed for things it wasn’t designed for - chronic back pain, insomnia, even mild anxiety. Many prescriptions came from primary care doctors, not neurologists or pain specialists. And many women were never told about the risks.
Now, awareness is growing. But many hospital protocols are still outdated. A 2023 survey found nearly half of U.S. neurology clinics hadn’t updated their pregnancy guidelines since 2018. That’s dangerous. We can’t rely on old assumptions.
What’s Next?
The FDA now requires manufacturers to track 5,000 pregnancy outcomes by 2027. That’s a big step. Meanwhile, a long-term study tracking 1,200 children exposed to gabapentin in utero is already underway, with results expected in late 2025. Will these kids have learning delays? Behavioral issues? Motor problems? We don’t know yet.
What we do know is this: gabapentinoids aren’t harmless. They’re not the same as a prenatal vitamin. They’re powerful drugs that cross the placenta and affect developing nerve cells. For some women, the benefits outweigh the risks. For others, they don’t. The key is making an informed choice - not a default one.
If you’re pregnant or planning to be, and you’re on gabapentin or pregabalin, talk to your doctor. Don’t stop cold turkey. Don’t assume it’s safe because your friend took it. Ask: Is this the best option for me? Are there alternatives? What’s the real risk to my baby? And if we keep using it, what monitoring will we need?
The answer won’t be easy. But it’s worth having.
Is gabapentin safe to take while pregnant?
Gabapentin is not considered completely safe during pregnancy. While it doesn’t significantly increase the overall risk of major birth defects, it’s linked to higher rates of preterm birth, babies being small for gestational age, and NICU admissions. There’s also a small but real increased risk of certain heart defects. It should only be used if other treatments have failed and the benefit to the mother clearly outweighs the potential risks to the baby.
Can gabapentin cause birth defects?
Overall, gabapentin does not appear to cause a large increase in major birth defects. The absolute risk rises only slightly - from about 3% to 3.7%. But there is a specific concern: conotruncal heart defects, a group of serious heart abnormalities. Studies show a 40% higher risk when gabapentin is taken regularly during the first trimester. While the absolute risk is still low (less than 1%), this signal is strong enough to warrant a fetal echocardiogram if the drug is used during pregnancy.
What are the risks of taking gabapentin in the third trimester?
Taking gabapentin late in pregnancy carries the highest risk for neonatal complications. Studies show that 38% of babies exposed until delivery need NICU care - compared to just 3% in unexposed babies. These infants often show signs of withdrawal: tremors, irritability, poor feeding, and breathing problems. This is not full opioid withdrawal, but it’s serious enough to require hospital monitoring. Avoiding gabapentin in the last few weeks of pregnancy can significantly reduce this risk.
Is pregabalin safer than gabapentin during pregnancy?
No, pregabalin is not safer. In fact, animal studies show stronger signs of developmental harm, and early human data suggests it may carry higher risks than gabapentin for birth defects and NICU admissions. Regulatory agencies like the European Medicines Agency now recommend avoiding pregabalin in pregnancy unless there’s no alternative. Many doctors are already reducing or stopping pregabalin use in pregnant patients in favor of gabapentin or non-drug treatments.
What should I do if I’m pregnant and taking gabapentin?
Do not stop taking gabapentin suddenly - this can trigger seizures or severe pain rebound. Talk to your doctor immediately. Together, review why you’re on it, whether the dose is the lowest possible, and whether alternatives exist. If you’re in the first trimester, discuss fetal echocardiography. If you’re in the third trimester, talk about tapering off safely before delivery. Your care team should include an obstetrician, a neurologist or pain specialist, and possibly a pharmacist with expertise in pregnancy.
Are there safer alternatives to gabapentin for pain during pregnancy?
Yes. For nerve pain, options include physical therapy, acupuncture, and cognitive behavioral therapy. Medications like duloxetine are sometimes used and have better safety data in pregnancy than gabapentinoids. For other types of pain, acetaminophen (paracetamol) is generally considered safe in moderation. Non-drug approaches should always be tried first. Gabapentin should only be used when these fail and the pain is severe enough to impact the mother’s health or ability to care for herself.





Write a comment
Your email address will be restricted to us