When you take a medicine, you expect it to work - not make you sicker. But with narrow therapeutic index drugs, even a tiny change in dose can turn treatment into danger. These aren’t ordinary pills. They sit on a razor’s edge: too little, and they don’t work. Too much, and they can land you in the hospital - or worse.
What exactly is a narrow therapeutic index drug?
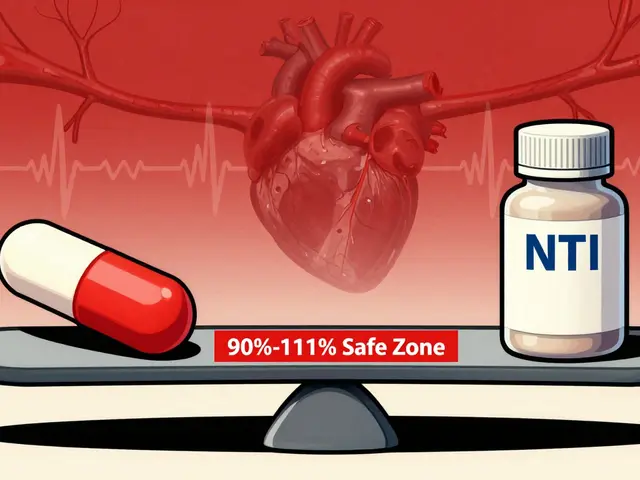
A narrow therapeutic index (NTI) drug means there’s almost no room for error. The difference between the dose that helps you and the dose that harms you is incredibly small. Think of it like walking a tightrope. One misstep, and you fall.
The U.S. Food and Drug Administration (FDA) defines NTI drugs as those where even small changes in blood levels can cause serious problems - like life-threatening bleeding, organ rejection, seizures, or heart rhythm issues. For most medicines, your body can handle a bit of variation. Not with NTI drugs. A 10-20% increase in concentration can push you from safe to toxic.
These drugs have been studied since the 1970s. Back then, scientists realized some medications didn’t follow the usual rules. A little more didn’t just mean a little better - it meant danger. Today, we know that NTI drugs require strict control. That’s why they’re monitored closely and why switching brands can be risky.
Common NTI drugs you might be taking
You might not realize you’re on one of these drugs - until something goes wrong. Here are the most common ones:
- Warfarin (Coumadin, Jantoven): Used to prevent blood clots. Too high? Risk of internal bleeding. Too low? Clots can form - leading to stroke or heart attack. Your INR must stay between 2.0 and 3.0. A jump to 4.0 or higher is an emergency.
- Lithium (Lithobid): For bipolar disorder. Therapeutic range? 0.6 to 1.2 mmol/L. Above 1.5? You could start shaking, feeling confused, or even have seizures.
- Levothyroxine (Synthroid): For hypothyroidism. Even a small switch in generic brands can cause your TSH levels to swing wildly - from normal to severely underactive in just weeks.
- Digoxin (Lanoxin): For heart failure and irregular heartbeat. Safe range: 0.5-0.9 ng/mL. Above 2.0? Life-threatening heart rhythms can occur.
- Tacrolimus (Prograf): After a transplant. Too low? Your body rejects the new organ. Too high? Your kidneys get damaged.
- Phenytoin (Dilantin) and Carbamazepine (Tegretol): For seizures. Small changes can trigger more seizures or cause dizziness, nausea, or even coma.
- Methotrexate (Trexall): Used for autoimmune diseases and some cancers. Even small overdoses can cause severe bone marrow suppression.
These aren’t rare. Millions of people take them. But few know how delicate their balance really is.
Why switching generics can be dangerous
Pharmacists often swap brand-name drugs for cheaper generics. That’s fine for most medicines. But with NTI drugs, it’s not that simple.
Even if two pills have the same active ingredient, the fillers, coatings, and how they dissolve in your body can differ slightly. For NTI drugs, those tiny differences matter. A 2021 study found patients who switched between generic versions of NTI drugs were 2.3 times more likely to be hospitalized for complications than those who stayed on the same product.
One patient on warfarin switched from brand Coumadin to a generic and saw their INR jump from 2.5 to 4.1 in just one week. That’s a dangerous spike. Emergency vitamin K was needed to reverse the bleeding risk.
In the U.S., the FDA doesn’t require generics for NTI drugs to prove they’re as close as the original - but many states, like North Carolina, now require pharmacists to get your doctor’s permission before switching. The European Medicines Agency (EMA) takes it further: for NTI drugs, they demand a tighter bioequivalence range (90-111%) compared to the standard 80-125% used for other drugs.
Bottom line: Don’t assume generics are interchangeable. Talk to your doctor before any switch.

Monitoring is non-negotiable
If you’re on an NTI drug, regular blood tests aren’t optional - they’re your safety net.
- Warfarin: INR tests every 1-4 weeks, especially when starting or changing doses.
- Lithium: Blood levels checked every 3-6 months, or more often after a dose change.
- Tacrolimus: Twice-weekly checks right after transplant, then gradually spaced out.
- Levothyroxine: TSH levels tested every 6-8 weeks after a dose change, then every 6-12 months if stable.
These tests aren’t just routine. They’re how your doctor knows whether you’re on the tightrope - or about to fall off.
Patients who keep a simple medication diary - noting doses, symptoms, and lab results - have 32% fewer bad events, according to the American College of Clinical Pharmacy. Write down how you feel. Track your test results. Bring it to every appointment.
What to watch for - signs of too much or too little
You don’t always need a blood test to know something’s wrong. Your body talks. Learn its language.
For warfarin:
- Too little: New swelling in your leg, chest pain, sudden shortness of breath (signs of a clot).
- Too much: Unexplained bruising, nosebleeds that won’t stop, red or dark urine, vomiting blood.
For lithium:
- Too little: Return of mood swings, depression, or mania.
- Too much: Tremors, slurred speech, confusion, dizziness, frequent urination, nausea.
For levothyroxine:
- Too little: Fatigue, weight gain, cold intolerance, brain fog.
- Too much: Rapid heartbeat, anxiety, weight loss, trouble sleeping, sweating.
These aren’t guesses. These are red flags backed by real patient experiences and clinical data. If you notice them, call your doctor - don’t wait.
Food, supplements, and other drugs can change everything
NTI drugs don’t live in a bubble. What you eat, what you take, even what you drink can interfere.
Warfarin is especially sensitive:
- Leafy greens (kale, spinach, broccoli) are high in vitamin K - they can make warfarin less effective.
- Alcohol can increase bleeding risk.
- Some antibiotics and painkillers (like ibuprofen) can dangerously raise your INR.
Lithium levels rise if you become dehydrated - so drink water, especially in hot weather or when you’re sick.
Levothyroxine should be taken on an empty stomach, at least 30-60 minutes before breakfast. Calcium, iron, and soy can block its absorption if taken too close together.
Always tell your doctor and pharmacist about every supplement, herb, or over-the-counter medicine you take. Even something as simple as a multivitamin can throw off your balance.

What’s changing in 2026 - and what it means for you
The rules are getting stricter - and that’s good news.
In 2023, the FDA released new guidance requiring specific bioequivalence tests for 15 NTI drugs, including levothyroxine and digoxin. They’re also rolling out barcode scanning in hospitals for 12 high-risk NTI drugs to prevent dosing errors.
And the biggest shift coming? Genetic testing. Researchers have found that your genes affect how you process drugs like warfarin and lithium. Variants in the CYP2C9 and VKORC1 genes explain up to 60% of why some people need much higher or lower doses than others.
By 2026, genetic testing before starting these drugs may become standard. It won’t eliminate monitoring - but it could cut down the trial-and-error period and reduce bad reactions by up to 35%.
Pharmacists are also being trained to recognize NTI drugs at the counter. Some states now require special counseling when these prescriptions are filled.
Your action plan: Stay safe with NTI drugs
If you take one of these drugs, here’s what you need to do - right now:
- Know your drug. Is it on the NTI list? Ask your doctor or pharmacist.
- Stick to one brand. Don’t let your pharmacy switch it without your doctor’s approval.
- Never skip blood tests. Treat them like appointments with your life.
- Track your symptoms. Keep a notebook: what you took, how you felt, when you had tests.
- Know the warning signs. Learn what too much or too little feels like for your specific drug.
- Tell everyone. Your dentist, ER staff, even your yoga instructor - if they’re giving you something new, ask if it interacts with your NTI drug.
NTI drugs aren’t scary because they’re dangerous. They’re dangerous because they’re misunderstood. With the right knowledge and habits, you can live safely on them - for years, even decades.
One patient on lithium told Reddit: ‘Regular blood tests kept me stable for 8 years. Before that, I was hospitalized three times in two years.’ That’s the difference awareness makes.
Are all generic drugs unsafe for NTI medications?
No, not all generics are unsafe. But some can cause problems because of small differences in how they’re made. For NTI drugs, even tiny variations in absorption can change your blood levels enough to cause harm. That’s why many doctors and pharmacists prefer you stay on the same brand or generic version - and why some states require your doctor to approve any switch.
Can I stop taking my NTI drug if I feel fine?
Never stop without talking to your doctor. These drugs often control serious conditions like heart rhythm, seizures, or thyroid function. Stopping suddenly can cause rebound effects - like a stroke, seizure, or thyroid crisis - even if you feel okay. Your body has adapted to the medication. Stopping it is like pulling the plug on a system that’s been running for months or years.
Why do I need blood tests so often?
Because your body’s response to NTI drugs isn’t predictable. Factors like diet, stress, illness, other medications, and even changes in your liver or kidney function can shift how the drug works. Blood tests give your doctor real-time data - not guesses. Without them, you’re flying blind.
Is there a list of all NTI drugs?
The FDA doesn’t publish an official list, but experts agree on the most common ones: warfarin, lithium, levothyroxine, digoxin, tacrolimus, phenytoin, carbamazepine, and methotrexate. DrugBank and clinical guidelines from the FDA and EMA are the best sources. If your drug requires regular blood monitoring, it’s very likely an NTI drug.
Will insurance cover the cost of frequent blood tests?
Yes, most insurance plans cover monitoring for NTI drugs because it prevents costly hospitalizations. If you’re being asked to pay out-of-pocket for regular INR or lithium tests, ask your doctor to write a letter of medical necessity. These tests are not optional - they’re essential for safety.
What’s next?
If you’re on an NTI drug, your next step isn’t to panic - it’s to get organized. Write down your drug, your target levels, your warning signs, and your next blood test date. Keep that list in your wallet or phone. Share it with a family member.
Ask your doctor: ‘Is this an NTI drug? Do I need to avoid switching generics? How often should I be tested?’ Don’t be shy. These questions save lives.
By 2026, genetic testing will make managing these drugs even safer. But until then, your awareness is the best tool you have. You’re not just taking a pill. You’re managing a delicate balance - and you’re the one who holds the scale.




Write a comment
Your email address will be restricted to us