Key Takeaways
- abiraterone can lower testosterone and estrogen levels, leading to reduced libido and erectile challenges.
- Fertility decline is common, but sperm banking before treatment preserves future family‑planning options.
- Side‑effects vary with age, baseline hormone levels, and concurrent androgen‑deprivation therapy (ADT).
- Management includes dose adjustments, hormone replacement, and counseling.
- Regular monitoring of hormone panels and sexual health questionnaires helps catch problems early.
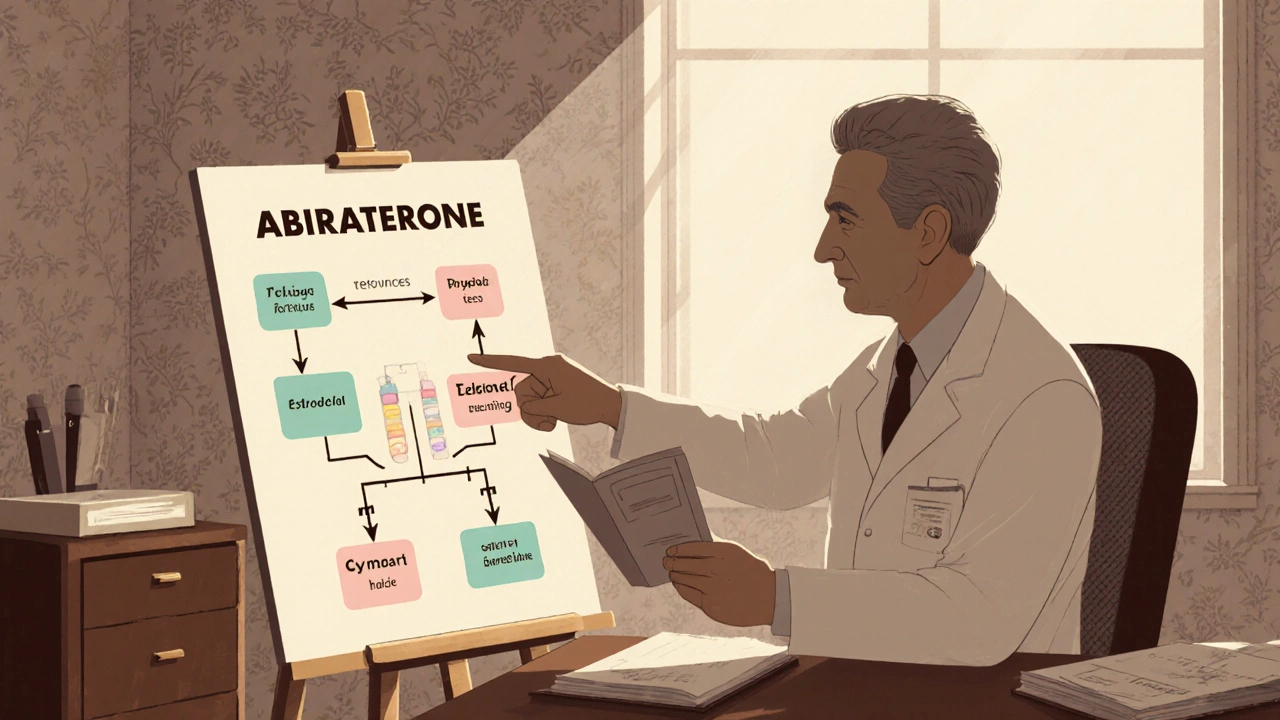
When a man receives a diagnosis of prostate cancer, the conversation quickly turns to treatment options and their side‑effects. One medication that appears on many oncologists’ prescribing lists is Abiraterone, a CYP17A1 inhibitor that blocks androgen production not only in the testes but also in the adrenal glands and tumor tissue. While the drug’s ability to prolong survival is well documented, patients often wonder how it will affect their sexual life and chances of fathering children. This guide breaks down the hormone changes, the real‑world impact on libido and erectile function, and practical steps to protect fertility when using abiraterone.
How Abiraterone Works: Hormone Mechanics in Simple Terms
Prostate cancer cells thrive on androgens-primarily testosterone and its more potent derivative dihydrotestosterone (DHT). Standard Androgen Deprivation Therapy (ADT) lowers circulating testosterone by either surgical castration or medication that suppresses the pituitary‑testicular axis. Abiraterone adds another layer by inhibiting the enzyme CYP17A1, which is crucial for converting cholesterol into both testosterone and estrogen in the adrenal glands and the tumor itself.
The result is a profound drop in serum testosterone-often below 20 ng/dL-and a simultaneous reduction in estradiol. Both hormones play key roles in sexual desire, erectile tissue health, and sperm production. Understanding these pathways helps explain why men on abiraterone frequently report a trio of symptoms: lower libido, difficulty achieving or maintaining an erection, and a decline in sperm count.
Sexual Function: What Patients Actually Experience
Clinical trials and real‑world registries give us a clear picture of how sexual health changes over the first six months of abiraterone therapy.
- Libido: Approximately 45‑55 % of men notice a marked decrease in sexual desire within three months. The drop correlates with estradiol levels falling below 10 pg/mL.
- Erectile Dysfunction (ED): Up to 38 % develop new‑onset ED. Low testosterone reduces nitric oxide production, a molecule essential for vasodilation in the penis.
- Orgasmic changes: Some patients report less intense orgasms or a feeling of “dryness,” likely linked to reduced seminal fluid volume.
It’s worth noting that the severity of these symptoms often improves after the first year, especially if hormone levels are stabilized with low‑dose glucocorticoids (prednisone 5 mg twice daily) that are co‑prescribed with abiraterone to mitigate mineralocorticoid excess.
Fertility Impact: From Sperm Production to Long‑Term Viability
Male fertility hinges on three factors: sperm count, motility, and morphology. Abiraterone’s suppression of testosterone disrupts the entire spermatogenic process, which normally requires a testosterone concentration of at least 300 ng/dL within the seminiferous tubules.
Studies measuring semen parameters before and after six months of abiraterone show:
| Parameter | Baseline | 6 Months | Change |
|---|---|---|---|
| Sperm concentration (million/mL) | 55 | 12 | ‑78 % |
| Total motility (%) | 68 | 42 | ‑38 % |
| Normal morphology (%) | 8 | 4 | ‑50 % |
Even though some men regain partial sperm output after stopping abiraterone, the recovery can take 12‑18 months and is not guaranteed. This makes proactive fertility preservation a critical discussion point before therapy begins.
Preserving Fertility: Real‑World Strategies
For patients who still want children, several options exist:
- Sperm Cryopreservation: The gold standard. Men can bank several vials before starting abiraterone. Success rates for later intracytoplasmic sperm injection (ICSI) are comparable to fresh samples if the sperm quality is adequate.
- Testicular Sperm Extraction (TESE): For men with very low ejaculate sperm counts, a minor surgical procedure can retrieve sperm directly from the testes.
- Hormone‑Supported Recovery: After completing abiraterone, clinicians sometimes prescribe low‑dose testosterone gel (e.g., 1‑2 g daily) for a limited period to jump‑start spermatogenesis, monitoring closely for cancer recurrence.
- Alternative Hormonal Regimens: In select cases, oncologists may opt for newer androgen‑receptor blockers (e.g., enzalutamide) that have a milder impact on estradiol, preserving some libido while still providing disease control.
All strategies require a coordinated approach involving the oncologist, a reproductive urologist, and often a mental‑health professional to address the emotional weight of fertility decisions.
Managing Sexual Side‑Effects: Practical Tips for Patients and Partners
Sexual health is not just a physical issue; it’s deeply tied to intimacy and self‑esteem. Here are evidence‑based tactics that have helped men maintain a satisfying sex life while on abiraterone:
- Hormone Replacement: Low‑dose testosterone (often < 100 ng/dL systemic levels) can be considered if cancer is well‑controlled, but this needs rigorous monitoring with PSA and imaging.
- Phosphodiesterase‑5 Inhibitors: Medications like sildenafil or tadalafil improve erectile function in 70‑80 % of treated men, even when testosterone is low.
- Psychosexual Counseling: Sessions with a therapist familiar in oncology care reduce anxiety and improve communication between partners.
- Lifestyle Adjustments: Regular exercise, a Mediterranean‑style diet, and stress‑reduction techniques (e.g., mindfulness) support overall hormonal balance.
- Alternative Intimacy Practices: Focusing on non‑penetrative activities can keep intimacy alive while physical changes resolve.
Any pharmacologic change, especially testosterone supplementation, must be cleared by the treating oncologist to avoid fueling cancer growth.
Monitoring Hormone Levels and Sexual Health: A Checklist
Proactive monitoring catches problems before they become entrenched. Use the following schedule as a guideline:
- Baseline labs: total testosterone, free testosterone, estradiol, LH, FSH, PSA.
- Month 1: Repeat testosterone and estradiol; administer a validated sexual function questionnaire (e.g., International Index of Erectile Function).
- Every 3 months: Full hormone panel, PSA, and symptom review.
- Every 6 months: Semen analysis if fertility preservation is a goal.
- At any sign of worsening sexual function: Offer PDE‑5 inhibitor trial and consider low‑dose testosterone under strict oncologic supervision.
Documenting trends helps the care team adjust the prednisone dose, explore alternative agents, or refer to a fertility specialist promptly.
When to Consider Alternative Therapies
Not every patient tolerates abiraterone’s sexual side‑effects. Decision points include:
- Persistent severe ED despite PDE‑5 inhibitors.
- Unmanageable loss of libido that harms relationship quality.
- Desire for paternity within a short time frame (<12 months) without sperm banking.
In such scenarios, switching to a non‑steroidal androgen‑receptor blocker (e.g., apalutamide) or enrolling in a clinical trial for novel agents may provide disease control with a milder sexual profile.
Bottom Line: Balancing Cancer Control and Quality of Life
Abiraterone offers a powerful weapon against advanced prostate cancer, but its hormone‑suppressing action can significantly affect sexual desire, erectile ability, and sperm production. The good news is that many of these effects are predictable, monitorable, and, in most cases, manageable with a blend of medication adjustments, fertility preservation techniques, and psychosocial support. Early conversations with the oncology team-ideally before the first dose-set the stage for informed choices and a smoother journey through treatment.
Can abiraterone cause permanent infertility?
Infertility is often reversible once the drug is stopped, but recovery can take 12‑18 months and is not guaranteed. Cryopreserving sperm before treatment is the most reliable way to ensure future paternity.
Is testosterone replacement safe while on abiraterone?
Low‑dose testosterone may improve libido and erectile function, but it must be prescribed only after careful oncologic review because it could stimulate residual cancer cells. Regular PSA monitoring is essential.
How long should I take prednisone with abiraterone?
Standard protocols use prednisone 5 mg twice daily for the entire course of abiraterone to counteract mineralocorticoid excess. Some clinicians taper the dose after 6‑12 months if side‑effects subside, but any change requires oncologist approval.
What are the alternatives to abiraterone for men concerned about sexual health?
Non‑steroidal androgen‑receptor inhibitors such as enzalutamide, apalutamide, or darolutamide tend to have a less dramatic impact on estradiol and may preserve more libido. Discuss disease stage and side‑effect profiles with your urologist.
Should my partner be involved in the sexual health monitoring?
Yes. Open communication helps identify problems early and allows both partners to explore coping strategies together, from counseling to adjusting intimacy practices.




Write a comment
Your email address will be restricted to us