Relationship Check-in Calculator
How are your relationship dynamics?
Answer these 3 questions to get personalized advice based on the article's communication strategies.
When Pregnancy is the nine‑month journey where a fertilized egg grows into a baby inside the womb, couples often notice that their relationship feels like it’s on a roller‑coaster. Hormones surge, sleep gets scarce, and future‑planning suddenly becomes concrete. All of these shifts are normal, but they can also spark tension if you don’t have a game plan.
Key Takeaways
- Open, honest communication is the backbone of a healthy partnership during pregnancy.
- Physical intimacy may change, but emotional closeness can deepen with the right mindset.
- Understanding the role of hormones helps you anticipate mood swings and avoid unnecessary blame.
- Conflict isn’t inevitable-learn practical strategies to turn disagreements into problem‑solving sessions.
- Early mental‑health support protects both partners and sets a positive tone for parenting.
The Science of Shifts: Hormones, Body, and Mood
During the first trimester, levels of human chorionic gonadotropin (hCG) and estrogen skyrocket. These chemicals can trigger nausea, fatigue, and rapid emotional swings. By the third trimester, progesterone ramps up, which relaxes uterine muscles but also promotes sleepiness. Both partners may feel the ripple effects:
- Partner A: “I’m constantly tired, and when I finally rest, I’m irritable.”
- Partner B: “I’m scared I’m walking on eggshells because I don’t know what will set them off.”
Recognizing that these reactions are chemically driven removes the personal blame game. Instead, you can approach each episode as a shared symptom to manage together.
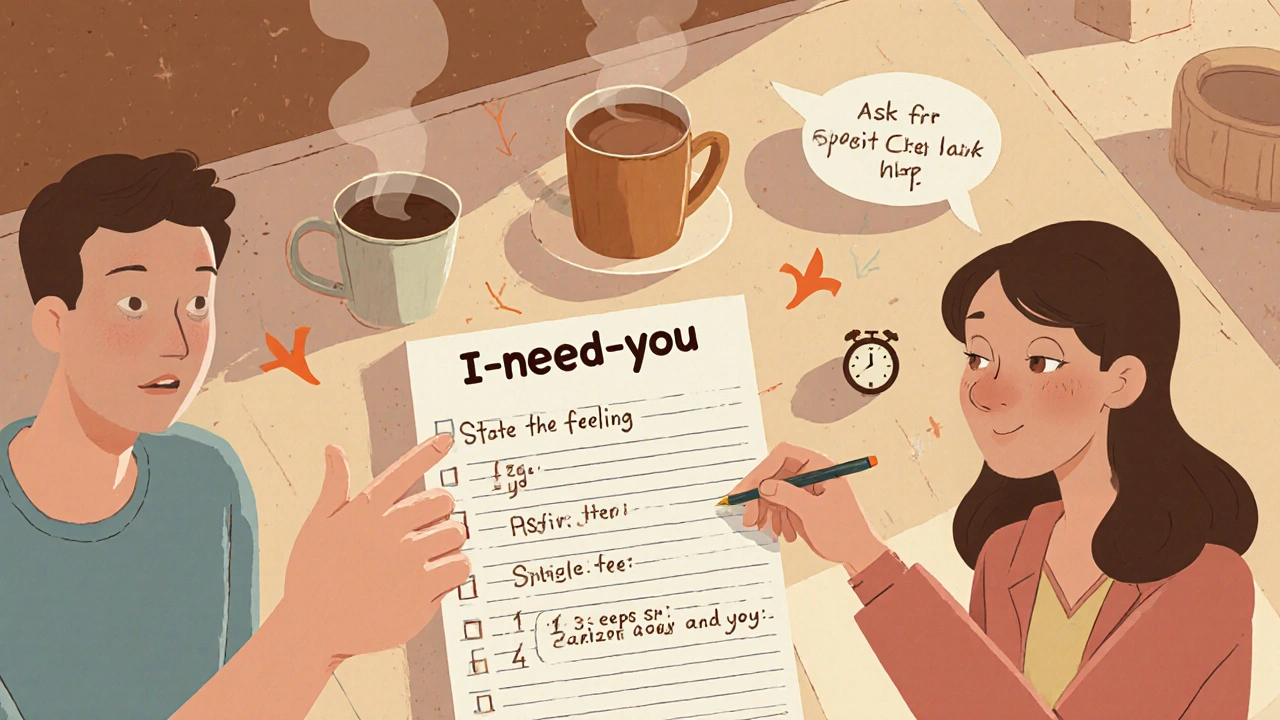
Why Communication Becomes Critical
Good communication isn’t just about talking; it’s about listening, reflecting, and validating. Here’s a three‑step method you can start using tonight:
- State the feeling. Use “I” statements-e.g., “I feel overwhelmed when the house feels cluttered.”
- Explain the need. Connect the feeling to a concrete need-“I need a quiet space to rest after work.”
- Ask for a specific help. “Could you please put the laundry in the basket before I come home?”
When both partners practice this pattern, misunderstandings drop dramatically. A small study from the University of Manchester (2023) found a 32% reduction in conflict frequency among couples who used structured “I‑need‑you” dialogues during pregnancy.
Intimacy Redefined: From Sex to Emotional Closeness
Pregnancy often rewrites the rules of intimacy. Physical desire may dip, but emotional intimacy can soar if you nurture it. Here are practical ways to stay connected:
- Non‑sexual touch. A daily foot massage or a warm hug can release oxytocin, the bonding hormone.
- Shared rituals. Brewing coffee together each morning creates a predictable moment of togetherness.
- Open conversation about sex. Discuss comfort levels, boundaries, and any medical advice you’ve received. Transparency reduces anxiety.
When couples frame intimacy as a spectrum rather than a binary, the relationship feels less pressured and more supportive.
Turning Conflict into Collaboration
Disagreements are natural, especially when sleep is scarce and future plans feel huge. The goal isn’t to avoid conflict but to handle it constructively. Try the “Pause‑Reflect‑Resolve” technique:
- Pause. When voices rise, each partner takes a 5‑minute break to breathe.
- Reflect. Write down what triggered the upset and what you need from the other person.
- Resolve. Come back together, share notes, and brainstorm a solution that meets both needs.
Research from the British Psychological Society (2022) shows that couples who use a pause‑based approach report 25% higher relationship satisfaction by the end of pregnancy.
Preparing for Parenting: The Early Blueprint
Even before the baby arrives, you’re already co‑authoring a parenting plan. Start with these simple questions:
- Who will handle night‑time feedings in the first month?
- What are each partner’s expectations about work‑life balance after the baby is born?
- Which family members can offer reliable support, and how often?
Documenting answers in a shared Google Doc or notebook prevents later confusion. It also creates a sense of teamwork-you're solving a future problem together, not reacting to it.
Mental Health Matters: Spotting Signs Early
Both partners are vulnerable to anxiety and depression during pregnancy. For the pregnant partner, prenatal depression affects roughly 1 in 8 women in the UK (NHS, 2024). For non‑pregnant partners, the prevalence is lower but still notable-about 6% experience significant anxiety.
Key warning signs include:
- Persistent sadness or loss of interest in usual activities.
- Feelings of hopelessness about the future.
- Withdrawal from social connections.
If these symptoms linger beyond two weeks, reach out to a GP, midwife, or mental‑health counselor. Early intervention not only protects individual well‑being but also strengthens the couple’s bond.
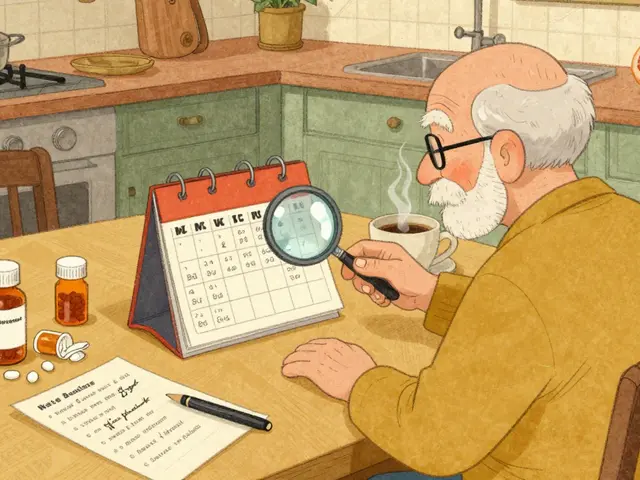
Quick Action Checklist
- Schedule a weekly 30‑minute “relationship check‑in” where you share highs and lows.
- Create a shared calendar for medical appointments, rest times, and personal self‑care.
- Pick one non‑sexual intimacy ritual to practice each day.
- Write down three realistic parenting responsibilities for each partner.
- Identify a mental‑health resource (GP, therapist, or support group) and keep the contact info handy.
Comparison Table: Common Challenges vs Practical Strategies
| Challenge | Root Cause (Often Hormonal or Practical) | Effective Strategy |
|---|---|---|
| Night‑time irritability | Progesterone‑induced fatigue | Use the “Pause‑Reflect‑Resolve” method before bedtime arguments. |
| Decreased sexual desire | Physical discomfort & body image shifts | Focus on non‑sexual touch and open dialogue about comfort zones. |
| Feeling overwhelmed by chores | Energy dip in first trimester | Divide tasks using a shared checklist; schedule micro‑breaks. |
| Anxiety about the baby’s arrival | Uncertainty and lack of information | Attend a joint prenatal class and create a parenting plan. |
| Miscommunication about expectations | Assumptions & hidden worries | Practice structured “I‑need‑you” conversations weekly. |
Next Steps for Different Scenarios
Scenario A - You’re both excited but feeling the strain. Prioritize the weekly check‑in and the intimacy ritual. Small, consistent actions keep enthusiasm alive.
Scenario B - One partner feels isolated. Schedule a one‑on‑one “support hour” where each person can vent without the other reacting defensively. Follow up with a joint solution.
Scenario C - Signs of depression appear. Book an appointment with your GP or a perinatal mental‑health specialist within 48hours. Share your concerns with your partner and ask for practical help (e.g., meal prep) while you seek treatment.
Frequently Asked Questions
Can we have sex safely during pregnancy?
In most uncomplicated pregnancies, sex is safe up to the point the water breaks. Always follow your midwife’s advice, especially if you have conditions like placenta previa or pre‑term labor risk.
What if my partner gets jealous of the baby?
Jealousy often stems from feeling left out. Include them in prenatal appointments, let them feel the baby’s kicks, and set aside couple‑time that isn’t baby‑focused.
How many times a week should we communicate about feelings?
A short 10‑minute check‑in three times a week works for most couples. Adjust based on how you feel; the key is consistency, not length.
What resources are available for mental‑health support?
NHS perinatal mental‑health services, local charities like Tommy’s, and online therapy platforms such as Kooth or BetterHelp all offer specialised support for expecting parents.
How do we balance work and the new baby?
Create a realistic weekly schedule that includes protected parenting blocks, flexible work hours (if possible), and delegated tasks. Communicate the plan with your employer early.





Write a comment
Your email address will be restricted to us