Knowing your risk for a heart attack or stroke isn’t just about guessing based on weight or family history. It’s about numbers-real, evidence-based numbers-that help doctors decide if you need medication, lifestyle changes, or both. The ASCVD score is one of the most trusted tools for this, used by doctors across the U.S. and increasingly in the UK and Europe. But it’s not perfect. And understanding how it works-and when to question it-can change your health outcomes.
What Exactly Is the ASCVD Score?
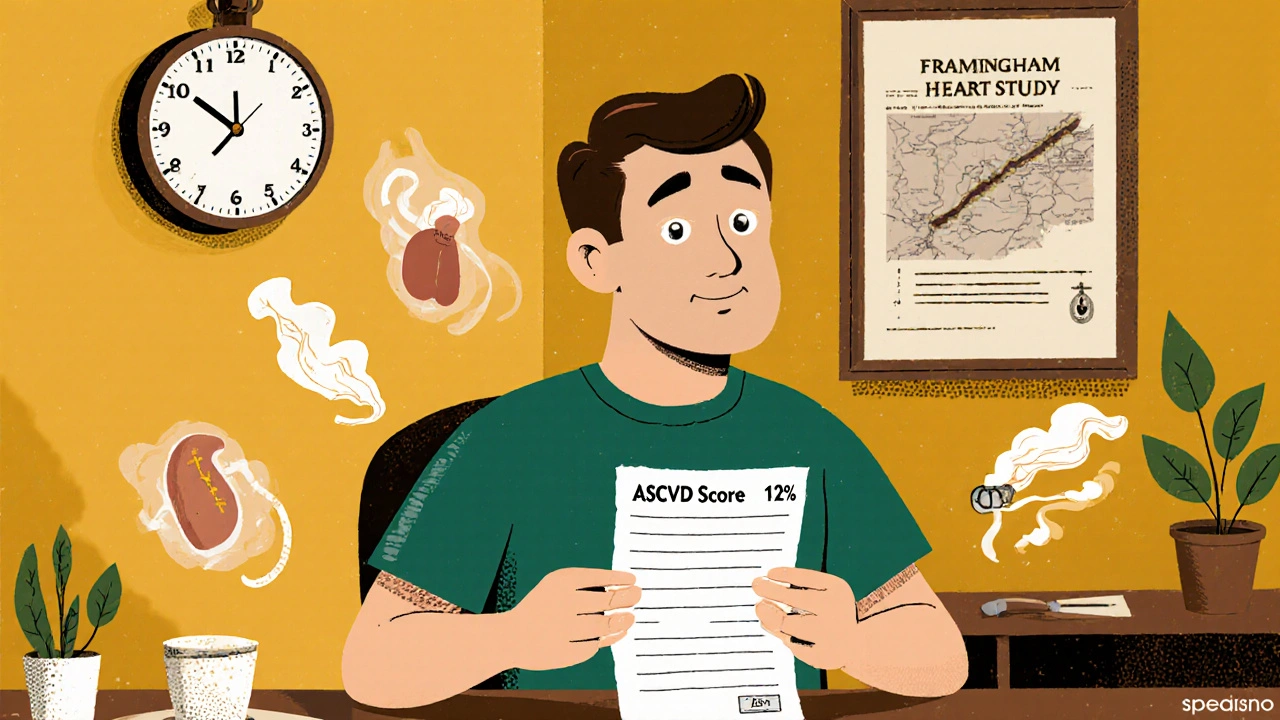
The ASCVD score stands for Atherosclerotic Cardiovascular Disease risk score. It estimates your chance of having a heart attack, stroke, or dying from heart disease in the next 10 years. It’s not a guess. It’s based on data from over 1.2 million people tracked for decades in major studies like the Framingham Heart Study and the Atherosclerosis Risk in Communities study. The math behind it was developed by 19 top cardiologists and published in 2013, with updates in 2018.
To calculate your score, you need nine things:
- Age (must be between 40 and 79)
- Sex
- Race (White, Black, Hispanic, or Asian)
- Total cholesterol
- HDL (good) cholesterol
- Systolic blood pressure
- Whether you take blood pressure meds
- Do you have diabetes?
- Do you smoke?
Plug those into the calculator, and it gives you a percentage. That number falls into one of four buckets:
- Low risk: under 5%
- Borderline: 5% to 7.4%
- Intermediate: 7.5% to 19.9%
- High risk: 20% or higher
If you’re in the high-risk group, guidelines say you should be on a high-intensity statin. At 7.5% or above, moderate-intensity statins are recommended for most adults without diabetes. But here’s the catch: this score was never meant to be the final word.
Why the ASCVD Score Can Be Misleading
One of the biggest problems with the ASCVD calculator is that it doesn’t work equally well for everyone. Studies show it underestimates risk by 15% to 25% in American Indians, South Asians, and Puerto Ricans. At the same time, it overestimates risk by 10% to 20% in East Asians and Mexican Americans. Why? Because the original data came mostly from White and Black populations in the U.S.-not enough from other groups.
That means a South Asian man in his 50s with normal cholesterol and blood pressure might have a 12% 10-year risk on the calculator-but his real risk could be closer to 18%. He might be told he doesn’t need a statin. But his actual risk is high enough that he should be.
And then there’s the issue of misreported data. People forget they smoke. They don’t know their exact cholesterol numbers. Blood pressure readings vary by 8 to 12 mm Hg depending on how and when they’re taken. One study found 22% of patients misreported their smoking status. That throws the whole calculation off.
Even doctors get it wrong. A 2016 study found that 31% of primary care physicians misclassified intermediate-risk patients as low risk. That’s dangerous. Intermediate risk is where decisions matter most.
What Do You Do If Your Score Is in the Middle?
Most people-about 35% to 40% of those aged 40 to 75-land in the intermediate-risk zone. That’s the gray area. The calculator can’t tell you whether to start a statin. That’s where doctors turn to other tests.
The most powerful next step? A coronary artery calcium (CAC) scan. This low-dose CT scan looks for actual calcium buildup in your heart’s arteries. It’s not a guess. It’s a direct picture of damage.
Here’s what happens when you add a CAC scan:
- If your CAC score is 0, your risk drops significantly-even if your ASCVD score says 15%. You’re likely safe without a statin.
- If your CAC score is over 100, your risk shoots up. Most doctors will start statins immediately.
- If it’s between 1 and 99, you’re still in the gray zone, but now you’ve got real data to guide the conversation.
One study found that CAC scoring changes treatment decisions in 68% of intermediate-risk patients. That’s huge. Another found that 52% of people in the intermediate group get reclassified to either low or high risk after the scan.
Other tests like high-sensitivity CRP (hsCRP) or ankle-brachial index (ABI) can help too. But CAC is the gold standard when the ASCVD score leaves you stuck.

Lifetime Risk Matters More Than You Think
The ASCVD score only looks 10 years ahead. But if you’re 45 and your 10-year risk is 8%, that doesn’t mean you’re safe. It means you’re on a path. Most heart events happen in people who never hit the 20% 10-year threshold.
That’s why doctors now look at lifetime risk too. If you’re under 55 and your 10-year risk is borderline or intermediate, your lifetime risk might be over 30%. That’s higher than many older people with high 10-year scores.
Think of it this way: a 48-year-old with a 7% 10-year risk but a 35% lifetime risk has more to lose than a 70-year-old with a 19% 10-year risk and a 40% lifetime risk. The younger person has more years to lose. Prevention matters more.
What About Newer Tools?
The ASCVD calculator is the standard, but it’s not the only game in town. The Reynolds Risk Score adds family history and a blood test for inflammation (hsCRP). It’s better at catching risk in people who seem low-risk by ASCVD standards.
The MESA score uses CAC data to give you a “coronary age.” A 55-year-old might have a coronary age of 78. That’s a wake-up call no percentage can match.
And now there’s something even newer: the American Heart Association’s PREVENT Online Calculator, launched in 2023. It doesn’t just look at cholesterol and blood pressure. It includes things like:
- Neighborhood poverty levels
- Food insecurity
- Access to healthy food
- Social isolation
Why? Because living in a food desert or a high-crime area raises your heart risk as much as smoking. These factors alone can increase your chance of dying from heart disease by 23%.
Even more exciting? The next generation of tools will use your DNA. A 2023 study in the UK Biobank showed that adding genetic data improved risk prediction by 14.3% in people with intermediate risk. We’re moving from clinical risk to genomic-clinical risk.
What Should You Do?
Don’t wait for your doctor to bring it up. Ask for your ASCVD score if you’re between 40 and 79. Get your numbers: total cholesterol, HDL, blood pressure, smoking status. Make sure they’re accurate.
If your score is low? Keep doing what you’re doing. Stay active. Eat real food. Don’t smoke.
If it’s high? Talk about statins. But also talk about why you’re at risk. Is it diet? Stress? Sleep? Genetics?
If it’s in the middle? Ask for a CAC scan. Don’t accept a statin prescription without it-or a refusal without it. You deserve to know what’s really going on in your arteries.
And if you’re South Asian, Indigenous, Puerto Rican, or from another group not well-represented in the original studies? Be extra cautious. Your score might be too low. Push for more testing. Your risk is real, even if the calculator doesn’t show it.
Final Thought: The Score Is a Conversation Starter, Not a Final Answer
The best cardiologists don’t treat the number. They treat the person. The ASCVD score is a tool to start a conversation-not to end it. It’s not a substitute for knowing your family history, your lifestyle, your stress levels, or your access to healthy food.
Doctors who rely only on the calculator miss the bigger picture. But doctors who use it as a map? They save lives.
Is the ASCVD calculator accurate for everyone?
No. The ASCVD calculator was built using data mostly from White and Black populations in the U.S. It underestimates risk by 15% to 25% in South Asians, American Indians, and Puerto Ricans. It overestimates risk in East Asians and Mexican Americans. If you’re from one of these groups, your score may not reflect your true risk. Ask for additional testing like a CAC scan.
What should I do if my ASCVD score is 12%?
A 12% 10-year risk puts you in the intermediate category. That’s the gray zone where decisions are hardest. You should ask for a coronary artery calcium (CAC) scan. If your CAC score is 0, you likely don’t need a statin. If it’s over 100, you probably do. The CAC scan will clarify your real risk.
Can I use the ASCVD calculator if I’m under 40?
The official ASCVD calculator only works for people aged 40 to 79. If you’re younger, your risk isn’t calculated the same way. But you can still assess your lifetime risk by looking at your cholesterol, blood pressure, smoking status, and family history. Early prevention-like eating well and staying active-is even more important for younger people with risk factors.
Do I need a statin if my ASCVD score is 8%?
Guidelines say yes, if you’re between 40 and 75 and don’t have diabetes. But this is where it gets personal. If you’re young, active, and have no other risk factors, your doctor might delay statins and focus on lifestyle. If you have a family history of early heart disease or a high CAC score, statins are strongly recommended. The score is a guide-not a rule.
Are there better tools than the ASCVD calculator?
Yes. The CAC scan is the most powerful next step for intermediate-risk patients. The Reynolds Risk Score adds inflammation and family history. The PREVENT calculator includes social factors like poverty and food access. And future tools will use genetic data. But none replace the ASCVD score as the starting point. They build on it.
How often should I get my ASCVD score recalculated?
If your risk is low and you’re healthy, every 4 to 5 years is fine. If you’re in the intermediate range, or if you’ve made lifestyle changes (like quitting smoking or losing weight), recalculate every 1 to 2 years. Your risk isn’t static. Your score shouldn’t be either.




Write a comment
Your email address will be restricted to us