When a limb is gone, the brain doesn’t always get the memo. For 60% to 85% of amputees, the pain doesn’t disappear with the limb-it lingers. Burning. Tingling. Cramping. As if the foot or hand is still there, twisted in agony. This isn’t imagination. It’s phantom limb pain, a real, measurable neurological condition rooted in the spinal cord and brain, not the mind.
Why Does Phantom Limb Pain Happen?
After an amputation, the nerves that once carried signals from the missing limb don’t just shut off. They keep firing. The brain, still expecting input from that area, interprets these random signals as pain. Neuroimaging studies show clear activity in the parts of the brain that used to control the lost limb-areas that now get rewired, often picking up signals from nearby body parts like the face or chest. That’s why touching your cheek might make your missing hand throb. This isn’t psychological. It’s physical. And it usually starts within days or weeks after surgery. For many, it fades. But if it lasts more than six months, the chances of it going away on its own are nearly zero. Without treatment, it can become a lifelong burden.Medications: The First Line of Defense
Most people start with medication. Not because it’s perfect, but because it’s fast, accessible, and often the only option offered early on. Tricyclic antidepressants like amitriptyline and nortriptyline are the most commonly prescribed. They’re not for depression here-they work on nerve pain. A typical starting dose is 10 mg at bedtime. That’s low. Doctors slowly increase it over weeks, watching for drowsiness, dry mouth, or dizziness. About 45% of users report moderate relief, but 60% quit because of side effects. Anticonvulsants like gabapentin and pregabalin are next. Gabapentin often starts at 300 mg a day and can go up to 3,600 mg. It helps 72% of users on Reddit’s amputee forum, but nearly 60% stop because of dizziness or brain fog. Pregabalin works similarly but can cause weight gain in 40% of users. For milder cases, over-the-counter NSAIDs like ibuprofen or naproxen offer short-term relief. But for most, their effect fades after three to six months. They don’t touch the nerve pain at its source. When nothing else works, doctors may turn to NMDA antagonists like ketamine, given intravenously. It’s powerful-some patients get 70% pain reduction-but it’s not for long-term use. Side effects include hallucinations, high blood pressure, and dissociation. Opioids like oxycodone or morphine are controversial. They’re used for severe cases, but the American Pain Society warns against daily doses over 50 morphine milligram equivalents. Long-term use leads to dependence in 35% of patients, according to PainManagement.org. They’re a last resort, not a solution.Mirror Therapy: Rewiring the Brain Without Pills
Mirror therapy is one of the most elegant non-drug treatments. It’s simple: place a mirror vertically so it reflects your intact limb, making it look like the missing one is still there. Then, you move both limbs-your real one and the one you see in the mirror-in sync. Your brain sees movement where there should be none. Slowly, it starts to unlearn the pain. It sounds too simple to work. But studies show it does. In clinical trials, 60-70% of patients who stick with it for 4-8 weeks report at least 50% pain reduction. The key? Consistency. You need 15 to 30 minutes a day, five to seven days a week. The problem? Most people quit. About 40% give up within eight weeks. It’s boring. It’s hard to stay motivated when you don’t feel immediate results. But for those who stick with it, the relief can last for months-even years. You don’t need fancy gear. A basic mirror box, made from a cardboard box and a mirror, costs under $20. Some hospitals provide them. Others sell them online. The real cost is time and patience.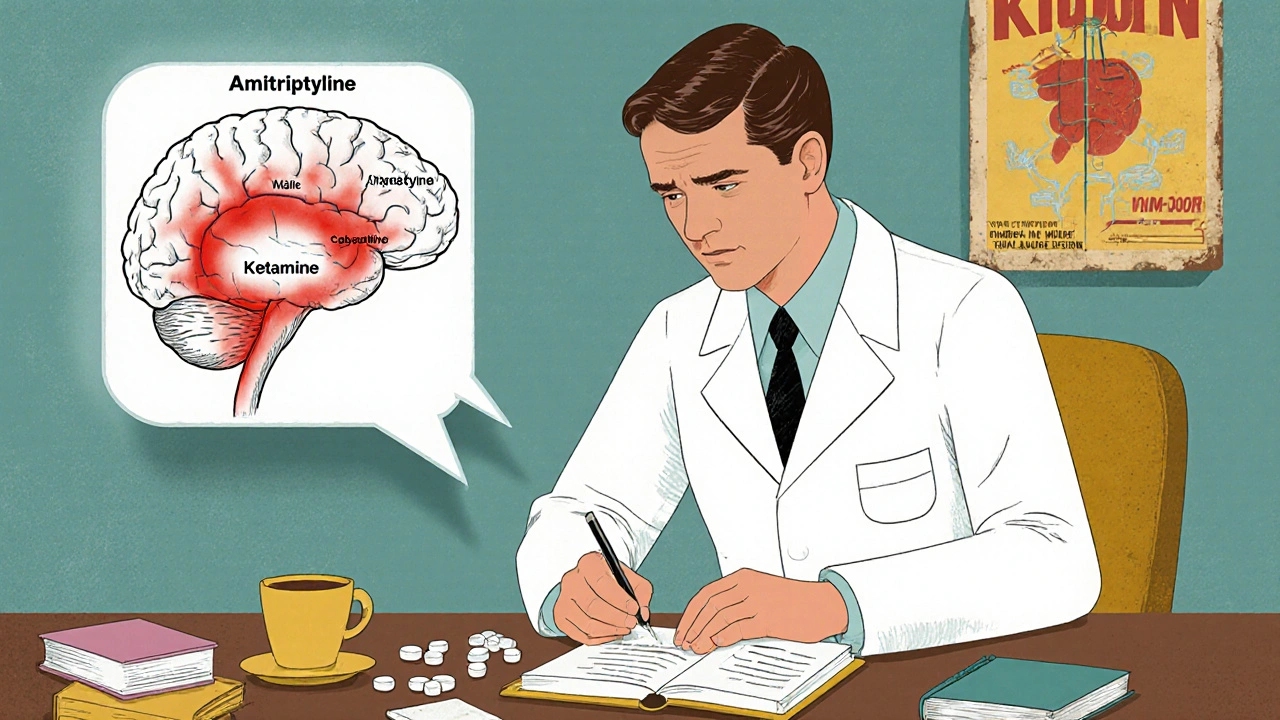
Other Non-Drug Options That Actually Work
Mirror therapy isn’t the only non-medication option. Transcutaneous Electrical Nerve Stimulation (TENS) uses small electrodes on the residual limb to deliver gentle pulses. It doesn’t fix the brain’s wiring, but it can block pain signals. Around 30-50% of users find it helpful, especially when combined with mirror therapy. TENS units are FDA-cleared, safe, and available over the counter. Botulinum toxin (Botox) injections into the residual limb can calm overactive nerves. In one 2023 case study, a patient’s pain dropped from 8/10 to 3/10 and stayed low for 12 weeks. It’s not for everyone-only those with neuromas or muscle spasms-but for some, it’s life-changing. Spinal cord stimulation involves implanting a device that sends electrical pulses to the spine. It’s invasive, expensive, and not for beginners. But for those with chronic, treatment-resistant pain, it works for 40-60% of users. The FDA approved a new closed-loop system in early 2024 that adjusts automatically to pain levels-showing 65% average reduction in trials. Biofeedback teaches you to control your body’s responses-heart rate, muscle tension-using real-time monitors. It’s not magic, but it gives you back some control. Studies show 25-40% effectiveness, and it’s low-risk.What Doesn’t Work (And Why)
Not every treatment you hear about is backed by science. Epidural anesthesia during surgery was once thought to prevent phantom pain. But research shows it doesn’t. The pain still comes. Acupuncture and herbal supplements have no strong evidence for PLP. Some people swear by them, but there’s no consistent data. Just waiting it out is the biggest mistake. If pain lasts beyond six months, it’s not going away without active treatment. The longer you wait, the harder it is to reverse the brain’s rewiring.
Combining Treatments: The Real Secret
No single treatment works for everyone. But when you combine them, results improve dramatically. A patient on gabapentin might add mirror therapy. Someone with muscle spasms might get Botox and use TENS. A person with severe pain might try spinal stimulation while tapering off opioids. The best outcomes come from multidisciplinary care: a pain specialist, physical therapist, and sometimes a psychologist working together. Hospitals with dedicated phantom limb pain clinics-now present in 68% of major U.S. centers-are seeing better long-term results.What to Do Next
If you or someone you know has phantom limb pain:- Start with a low-dose tricyclic antidepressant or gabapentin-talk to your doctor about side effects.
- Get a mirror box and try 15 minutes a day. Don’t expect miracles in a week. Give it 4-6 weeks.
- Try TENS if you’re not on meds yet. It’s safe and easy to start.
- Keep a pain journal. Note triggers: stress, weather, fatigue, ill-fitting prosthetics.
- Join a support group. The Amputee Coalition has over 12,000 members. Talking to others who get it makes a difference.
Frequently Asked Questions
Is phantom limb pain all in my head?
No. Phantom limb pain is a real neurological condition. Brain scans show activity in areas that once controlled the missing limb. It’s not psychological-it’s a result of nerve damage and brain rewiring after amputation.
How long does phantom limb pain last?
For some, it fades within weeks. But if it lasts more than six months, it’s unlikely to go away without treatment. The longer it persists, the more entrenched the brain’s pain signals become. Early intervention is key.
Can mirror therapy cure phantom limb pain?
It doesn’t cure it, but it can significantly reduce pain for many. Studies show 60-70% of people who stick with daily mirror therapy for 4-8 weeks get at least half their pain relief. It works by helping the brain unlearn the pain signal.
Are opioids safe for phantom limb pain?
Opioids can help with severe pain short-term, but they carry a high risk of dependence. The American Pain Society recommends limiting daily doses to under 50 morphine milligram equivalents. They’re not a long-term solution and should only be used when other treatments fail.
What triggers phantom limb pain?
Common triggers include stress, fatigue, pressure on the residual limb, cold weather, infection, and poorly fitting prosthetics. Keeping a pain journal helps identify your personal triggers so you can avoid them.
Can I do mirror therapy at home?
Yes. You can make a simple mirror box with a cardboard box and a mirror. Do 15-30 minutes a day, five to seven days a week. Many hospitals provide them for free. The hard part isn’t the equipment-it’s staying consistent.
Is there a cure for phantom limb pain?
There’s no single cure, but many people achieve long-term relief through combination therapy-medication, mirror therapy, TENS, and sometimes nerve stimulation. The goal isn’t to eliminate pain completely, but to reduce it enough to live well.



Write a comment
Your email address will be restricted to us