When a sexually active person gets an unexpected pelvic ache, fever, or abnormal discharge, doctors often think about pelvic inflammatory disease (PID). The big question is which antibiotic will clear the infection fast without causing a lot of side‑effects. One drug that keeps popping up in guidelines and clinic discussions is Ofloxacin. This article breaks down what Ofloxacin is, why it matters for PID, how it compares to other regimens, and what you should watch out for.
Key Points to Remember
- Ofloxacin is a fluoroquinolone that can target the common bacteria behind PID.
- Current WHO and CDC guidelines list Ofloxacin as an alternative when first‑line drugs can’t be used.
- Resistance, especially in Neisseria gonorrhoeae is the bacteria that causes gonorrhea and is a leading cause of PID, is the biggest downside.
- Typical adult dosing is 400 mg twice daily for 14 days, but the exact schedule can vary by country.
- Patients should be warned about tendon pain, photosensitivity, and potential drug interactions.
What Exactly Is Ofloxacin?
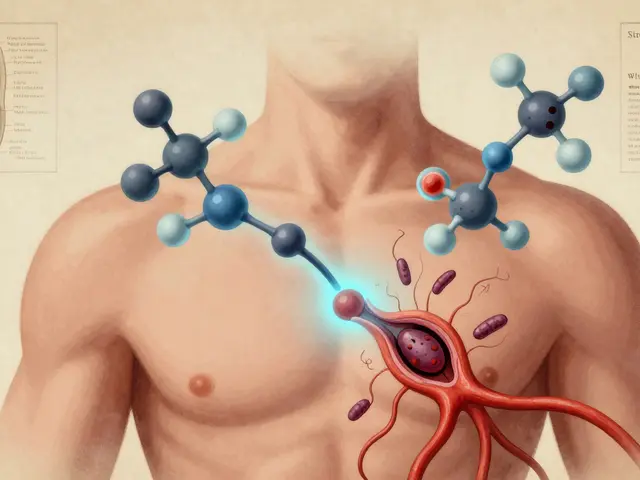
Ofloxacin is a broad‑spectrum fluoroquinolone antibiotic that interferes with bacterial DNA gyrase and topoisomerase IV, stopping DNA replication. First approved in the late 1980s, it’s been used for urinary‑tract infections, respiratory infections, and skin infections. Because it works well against gram‑negative rods and some atypical organisms, clinicians sometimes turn to it for complicated genital tract infections like PID.
How Pelvic Inflammatory Disease Develops
Pelvic Inflammatory Disease is an infection of the upper female reproductive organs-typically the uterus, fallopian tubes, and surrounding tissues. The infection usually starts in the lower genital tract and climbs upward. The most common culprits are Chlamydia trachomatis and the bacterium responsible for the most frequent sexually transmitted infections worldwide and Neisseria gonorrhoeae is the pathogen behind gonorrhea, another leading cause of PID. Emerging pathogens like Mycoplasma genitalium are also being recognized as contributors, especially in cases that don’t respond to standard therapy.
The infection can lead to chronic pelvic pain, infertility, and an increased risk of ectopic pregnancy. Prompt, effective antibiotic therapy is essential to stop the bacteria from damaging the delicate fallopian tubes.
Why Consider Ofloxacin for PID?
First‑line regimens recommended by the CDC is the U.S. Centers for Disease Control and Prevention, which issues treatment guidelines for sexually transmitted infections combine a third‑generation cephalosporin (like ceftriaxone) with doxycycline, sometimes adding metronidazole for anaerobes. However, there are scenarios where clinicians look for alternatives:
- Allergy or intolerance to β‑lactams (e.g., penicillin, cephalosporin).
- Co‑infection with organisms that need a fluoroquinolone’s broader spectrum.
- Geographic regions where local resistance patterns make ceftriaxone less reliable.
In those cases, Ofloxacin’s ability to hit both Neisseria gonorrhoeae and Chlamydia trachomatis with a single oral agent simplifies treatment, improves adherence, and reduces the need for injections.
Current Guidelines and Typical Dosing
The WHO guidelines is the World Health Organization's recommendations for the management of sexually transmitted infections list Ofloxacin 400 mg PO twice daily for 14 days as an alternative regimen for uncomplicated PID when first‑line therapy cannot be given. The CDC’s 2023 update mentions Ofloxacin as an acceptable oral option in the same dosing range, but stresses that local resistance data should drive the final choice.
Key dosing points:
- Adults: 400 mg every 12 hours for 14 days.
- Renal impairment: reduce dose to 200 mg every 12 hours if eGFR <30 mL/min.
- Pregnancy: Category C; avoid unless benefits outweigh risks.
Therapeutic drug monitoring isn’t routine, but clinicians should verify that the patient completes the full course to prevent relapse.
How Ofloxacin Stacks Up Against Other Regimens
| Regimen | Key Drugs | Duration | Advantages | Limitations |
|---|---|---|---|---|
| First‑line (CDC) | Ceftriaxone 250 mg IM + Doxycycline 100 mg PO BID | 14 days (doxycycline) | High efficacy, well‑studied | Injection required, β‑lactam allergy issues |
| Ofloxacin alternative | Ofloxacin 400 mg PO BID | 14 days | All‑oral, covers gram‑negatives and atypicals | Resistance in N. gonorrhoeae, tendon risk |
| Azithromycin + Metronidazole | Azithromycin 1 g PO single dose + Metronidazole 500 mg PO BID | 7 days (metronidazole) | Convenient dosing | Less effective against N. gonorrhoeae, rising macrolide resistance |
While the injection‑based regimen remains the gold standard, the Ofloxacin arm offers a practical option when logistics or allergies get in the way. The trade‑off is a higher chance of treatment failure if the local N. gonorrhoeae strain carries fluoroquinolone resistance.
Resistance and Safety Concerns
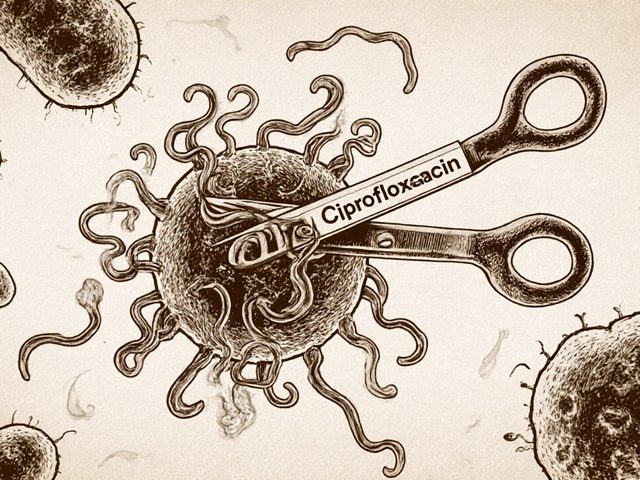
Fluoroquinolone resistance has surged over the past decade, especially in Neisseria gonorrhoeae is the bacterium that is increasingly resistant to many antibiotic classes, including fluoroquinolones. The CDC’s 2024 report shows that >30 % of isolates in the U.S. are non‑susceptible to ciprofloxacin, a close cousin of Ofloxacin. This makes susceptibility testing essential before committing to a fluoroquinolone‑only regimen.
Safety-wise, Ofloxacin shares the class‑wide warnings of tendon rupture, peripheral neuropathy, and photosensitivity. Elderly patients, those on corticosteroids, or people with a history of tendon disorders should avoid it. Drug interactions with antacids, warfarin, and certain anti‑arrhythmics (e.g., amiodarone) also need attention.
Practical Tips for Clinicians and Patients
- Check local resistance data before prescribing Ofloxacin as first‑line.
- Ask about allergies to β‑lactams; if present, Ofloxacin can be a reasonable fallback.
- Educate patients to report any sudden calf or Achilles pain - it could be a tendon issue.
- Advise on sun protection: Ofloxacin can increase UV sensitivity.
- Ensure the patient completes the full 14‑day course, even if symptoms improve early.
For women of child‑bearing age, discuss contraception options because the drug’s safety data in pregnancy are limited. Follow‑up visits at the end of therapy help confirm microbiological cure and catch any complications early.
Frequently Asked Questions
Can Ofloxacin be used as the sole treatment for PID?
Yes, when the patient cannot receive injectable cephalosporins or doxycycline, a 14‑day course of Ofloxacin 400 mg twice daily meets the WHO and CDC recommendations as an alternative. Success hinges on local susceptibility patterns.
What are the main side‑effects I should watch for?
Common issues include nausea, diarrhea, and mild headache. Rare but serious concerns are tendon rupture, peripheral neuropathy, and severe photosensitivity. Report any sudden joint or muscle pain right away.
Is fluoroquinolone resistance a deal‑breaker?
If local labs show >10 % resistance in N. gonorrhoeae, clinicians should avoid Ofloxacin and opt for the standard ceftriaxone‑based regimen. Resistance testing before treatment is ideal but not always available.
How does Ofloxacin interact with other meds?
Antacids containing magnesium or aluminum can cut absorption - take Ofloxacin at least two hours apart. Warfarin levels may rise, requiring closer INR monitoring. Certain anti‑arrhythmics (e.g., amiodarone) also need caution.
Can I take Ofloxacin while pregnant?
Ofloxacin is Category C; it’s not the first choice in pregnancy. Only use it if the benefits clearly outweigh the potential risks and no safer alternatives are available.
Bottom line: Ofloxacin is a solid backup for PID when first‑line drugs can’t be used, but its utility depends on resistance trends and patient‑specific risk factors. Keep an eye on local guidelines, talk openly with patients about side‑effects, and always complete the full course.






Write a comment
Your email address will be restricted to us