When you get a bad urinary tract infection, a stubborn sinus infection, or even a serious case of food poisoning, your doctor might reach for ciprofloxacin. It’s not a new drug, but it’s still one of the most common antibiotics used in clinics and hospitals today. Unlike painkillers that just hide symptoms, ciprofloxacin goes after the bacteria causing the problem. But how does it actually work? And when is it the right choice-or the wrong one?
What Ciprofloxacin Is and How It Works
Ciprofloxacin is a fluoroquinolone antibiotic that kills or stops the growth of certain bacteria. It was first approved in the 1980s and quickly became a go-to for infections that didn’t respond to older antibiotics like penicillin. It doesn’t just target one type of bug-it’s broad-spectrum, meaning it hits a wide range of bacteria, including Escherichia coli (E. coli), Salmonella, Shigella, and even some strains of Pseudomonas aeruginosa, which can cause dangerous hospital-acquired infections.
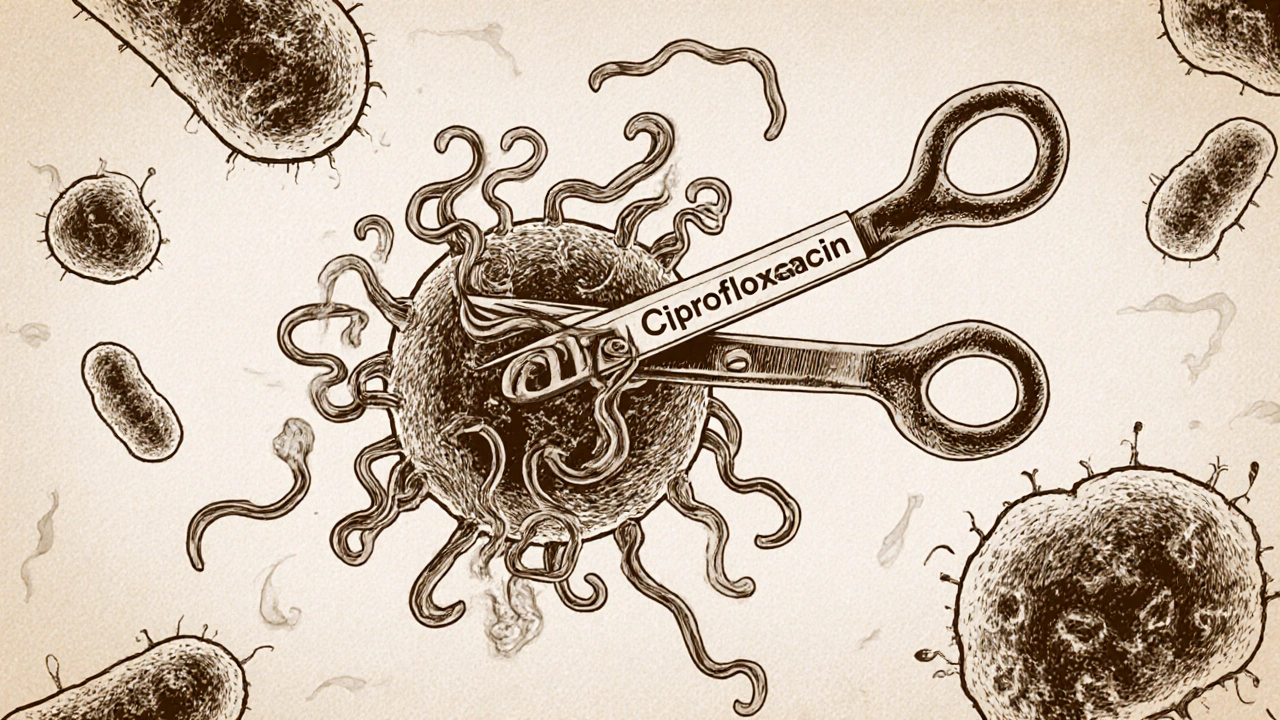
The way it works is simple but powerful. Bacteria need to copy their DNA to multiply. Ciprofloxacin blocks two key enzymes-DNA gyrase and topoisomerase IV-that act like molecular scissors and glue during this process. Without them, the bacteria can’t replicate. Their DNA gets tangled, they can’t divide, and they die off. This makes it especially effective against fast-growing infections.
Common Infections Treated with Ciprofloxacin
Not every infection needs ciprofloxacin. Doctors choose it based on the type of bacteria, the location of the infection, and whether other antibiotics have failed. Here are the most common uses:
- Urinary tract infections (UTIs): Especially complicated ones or those caused by drug-resistant E. coli. A 7-day course often clears it up.
- Respiratory infections: Like chronic bronchitis flare-ups or certain types of pneumonia, especially in people with weakened immune systems.
- Gastrointestinal infections: Traveler’s diarrhea caused by E. coli or Shigella. In outbreaks, it’s used to stop spread.
- Skin and soft tissue infections: When there’s a deep cut or wound infected with resistant bacteria.
- Bone and joint infections: Often used in combination with other drugs for osteomyelitis.
- Anthrax exposure: It’s one of the few antibiotics approved for post-exposure treatment after inhaling anthrax spores.
It’s rarely the first choice for simple strep throat or ear infections-that’s usually amoxicillin’s job. Ciprofloxacin is saved for when other options don’t work or when the infection is more serious.
Who Shouldn’t Take Ciprofloxacin
Just because it’s powerful doesn’t mean it’s safe for everyone. There are real risks.
The FDA issued strong warnings in 2016 and again in 2018 about the potential for serious side effects. These aren’t rare. In fact, studies show up to 1 in 10 people taking fluoroquinolones like ciprofloxacin report some form of adverse reaction. The biggest concerns:
- Tendon damage: Especially the Achilles tendon. It can rupture even in healthy people, sometimes weeks after stopping the drug. Risk goes up if you’re over 60, on steroids, or have kidney disease.
- Nerve damage (peripheral neuropathy): Tingling, burning, or numbness in hands and feet. This can be permanent.
- Central nervous system effects: Dizziness, confusion, hallucinations, or seizures in rare cases.
- Low blood sugar: Especially dangerous for diabetics on insulin or oral meds.
- Heart rhythm issues: Can prolong the QT interval, increasing risk of dangerous arrhythmias, especially if combined with certain heart meds.
It’s also not recommended for children under 18, except in life-threatening cases like anthrax or plague, because it can affect growing cartilage. Pregnant women should avoid it unless absolutely necessary-animal studies show harm to developing joints.

How It Compares to Other Antibiotics
There are dozens of antibiotics. Why pick ciprofloxacin over others?
| Antibiotic | Type | Best For | Key Risks | Oral Dosing |
|---|---|---|---|---|
| Ciprofloxacin | Fluoroquinolone | UTIs, GI infections, resistant Gram-negative bacteria | Tendon rupture, nerve damage, QT prolongation | Twice daily |
| Amoxicillin | Penicillin | Ear infections, strep throat, sinusitis | Allergic reactions, diarrhea | Three times daily |
| Trimethoprim-Sulfamethoxazole | Sulfonamide | Simple UTIs, some skin infections | Severe skin reactions, low blood cell counts | Twice daily |
| Levofloxacin | Fluoroquinolone | Pneumonia, sinusitis | Same as ciprofloxacin, slightly less GI upset | Once daily |
| Azithromycin | Macrrolide | Respiratory infections, STIs | Heart rhythm issues, stomach upset | Once daily, short course |
Levofloxacin is similar to ciprofloxacin but is often preferred for lung infections because it reaches higher concentrations in lung tissue. Amoxicillin is safer for most common infections and doesn’t carry the same long-term risks. That’s why guidelines now say: use ciprofloxacin only when no safer alternative exists.
What Happens If You Don’t Finish the Course?
One of the biggest problems with antibiotics today is resistance. When people stop taking ciprofloxacin early because they feel better, the toughest bacteria survive. These survivors multiply and pass on their resistance genes. Over time, that’s how superbugs emerge.
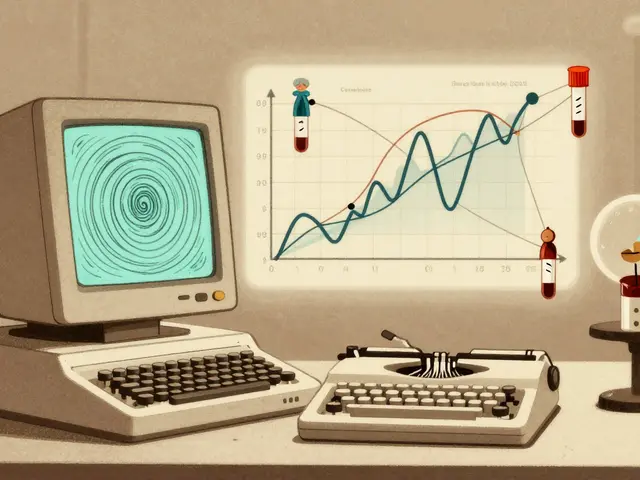
In the UK, the NHS tracks antibiotic resistance closely. As of 2025, about 15% of E. coli strains causing UTIs are resistant to ciprofloxacin-up from under 5% in 2010. That means if you’ve had a UTI before and were treated with ciprofloxacin, there’s a real chance it won’t work the next time.
Doctors now rely on urine cultures before prescribing ciprofloxacin for UTIs. If the lab shows resistance, they switch to nitrofurantoin or fosfomycin instead. This targeted approach slows down resistance.
What to Expect When Taking Ciprofloxacin
If your doctor prescribes it, you’ll typically get 250 mg to 750 mg twice a day, depending on the infection. Take it on an empty stomach-1 hour before or 2 hours after meals-because food, especially dairy, can block absorption. Antacids with magnesium or aluminum? Don’t take them within 6 hours of ciprofloxacin. Same with iron supplements or calcium-fortified juice.
Some side effects are common and harmless: nausea, diarrhea, headache. But if you feel sudden pain in your heel, or numbness in your fingers, stop taking it and call your doctor right away. Don’t wait. Tendon damage can happen fast.
Also avoid direct sunlight. Ciprofloxacin can make your skin more sensitive, leading to severe sunburn even after brief exposure. Wear sunscreen and cover up.
When Ciprofloxacin Isn’t the Answer
Many people assume antibiotics fix everything. They don’t. Ciprofloxacin does nothing against viruses-so it won’t help with colds, flu, or most sore throats. Using it unnecessarily increases your risk of side effects and contributes to resistance.
It’s also not ideal for:
- Strep throat (use penicillin or amoxicillin)
- Most sinus infections (they’re often viral)
- Simple bladder infections in young women (nitrofurantoin or trimethoprim are safer first choices)
- Infections caused by MRSA (it doesn’t work on this type of staph)
Doctors are getting better at choosing wisely. In Manchester’s NHS clinics, antibiotic prescribing for UTIs dropped by 22% between 2020 and 2025 because of stricter guidelines and better testing.
Alternatives to Ciprofloxacin
If you can’t take ciprofloxacin-or if it’s not working-there are other options:
- Nitrofurantoin: First-line for simple UTIs. Safe for most people, low resistance rates.
- Fosfomycin: Single-dose treatment for uncomplicated UTIs.
- Cephalexin: For skin infections or some respiratory bugs.
- Trimethoprim-sulfamethoxazole: Used when resistance to nitrofurantoin is high.
- Meropenem or piperacillin-tazobactam: IV antibiotics for severe hospital infections.
Doctors now use rapid diagnostic tests to identify the exact bacteria and its resistance profile within 24 hours. This means treatment can be tailored faster, reducing the need for broad-spectrum drugs like ciprofloxacin.
Final Thoughts: Use It Wisely
Ciprofloxacin is a powerful tool. It’s saved lives in outbreaks, treated deadly infections, and helped people recover when nothing else worked. But it’s not a magic bullet. Its risks are real, and overuse is making it less effective.
If your doctor prescribes it, ask: Why this one? Is there a safer option? What signs should I watch for? Take it exactly as directed. Don’t save leftover pills for next time. And never share antibiotics.
The goal isn’t just to kill the infection today-it’s to make sure ciprofloxacin still works for someone else tomorrow.
Can ciprofloxacin treat a cold or the flu?
No. Ciprofloxacin only works against bacterial infections. Colds and flu are caused by viruses, so antibiotics like ciprofloxacin won’t help and may cause unnecessary side effects or contribute to antibiotic resistance.
Is it safe to drink alcohol while taking ciprofloxacin?
There’s no direct dangerous interaction between alcohol and ciprofloxacin, but drinking can worsen side effects like dizziness, nausea, or liver stress. It’s best to avoid alcohol while on the medication and for a few days after.
How long does it take for ciprofloxacin to start working?
Most people start feeling better within 24 to 48 hours. But you must finish the full course-even if symptoms disappear-because the infection might not be fully cleared yet.
Can ciprofloxacin cause long-term damage?
Yes, in rare cases. Tendon rupture, nerve damage (peripheral neuropathy), and lasting joint or muscle pain can occur even after stopping the drug. These risks are higher in older adults, those on steroids, or with kidney problems. Always report unusual pain or numbness right away.
Why is ciprofloxacin not used for children?
Animal studies showed ciprofloxacin can damage developing cartilage in joints. It’s avoided in children under 18 unless it’s a life-threatening infection like anthrax or plague, where the benefits outweigh the risks.
What should I do if I miss a dose of ciprofloxacin?
Take it as soon as you remember, unless it’s almost time for your next dose. Never double up. If you’re unsure, call your pharmacist or doctor. Missing doses reduces effectiveness and increases resistance risk.
Does ciprofloxacin interact with other medications?
Yes. Avoid antacids, iron pills, calcium supplements, and zinc within 6 hours of taking ciprofloxacin. It also interacts with blood thinners like warfarin, some antidepressants, and heart rhythm drugs. Always tell your doctor what else you’re taking.




Write a comment
Your email address will be restricted to us