Diabetes Emergency Preparedness Check
Emergency Scenario Assessment
Answer these questions to determine the urgency and correct response for diabetes-related emergencies.
Emergency Kit Checklist
- Glucagon ready-to-use (Baqsimi/Gvoke) - Not checked
- Ketone test strips - Not checked
- Glucose tablets (15g) - Not checked
- Emergency contacts - Not checked
- Medical ID bracelet - Not checked
When your blood sugar drops too low or spikes too high because of diabetes medication, it’s not just a bad day-it’s a medical emergency. Every year, tens of thousands of people with diabetes end up in the hospital because of severe hypoglycemia or hyperglycemic crises. And too often, it’s preventable. The difference between life and death can come down to knowing what to do in the first five minutes.
What Counts as Severe Hypoglycemia?
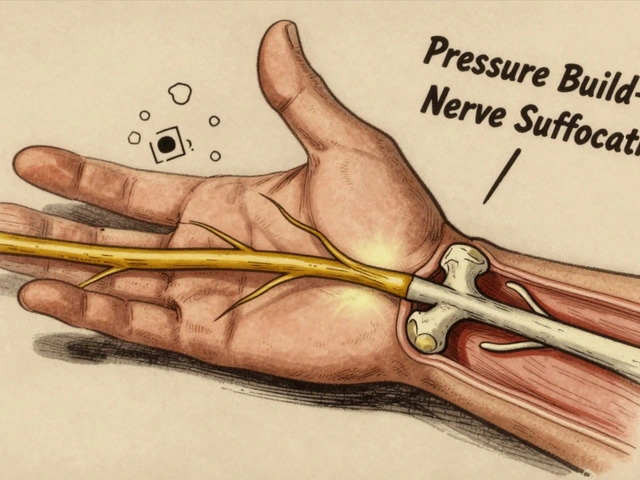
Severe hypoglycemia isn’t just feeling shaky or sweaty. It’s when your blood sugar falls below 54 mg/dL (3.0 mmol/L) and you’re too confused, weak, or unconscious to treat yourself. This happens most often with insulin or sulfonylureas-medications that force your body to lower blood sugar. A 2019 JAMA study found that people with type 1 diabetes have a 30% chance each year of experiencing a severe low that needs someone else to help.Here’s the scary part: if you don’t act fast, your brain starts shutting down. You might slur your words, collapse, or have a seizure. Untreated, severe hypoglycemia kills 6% of people within 24 hours. And most of these episodes happen at home, not in a clinic.
How to Treat Severe Hypoglycemia Right Now
If someone can’t swallow or is unconscious, don’t try to give them juice or candy. You could choke them. The only safe, proven fix is glucagon.Glucagon is a hormone that tells your liver to dump stored sugar into your bloodstream. For decades, the only option was a messy kit: freeze-dried powder you had to mix with liquid, then inject. Most people couldn’t do it-even trained nurses struggled. That’s why 95% of glucagon kits sat unused for years.
That changed in 2019. Two new options hit the market:
- Baqsimi: A nasal spray you just puff into the nose. No needles. No mixing.
- Gvoke: A pre-filled autoinjector you press against the thigh or arm. Works like an EpiPen.
Studies show 93% of people get a blood sugar boost within 15 minutes using these. One study found caregivers could administer nasal glucagon in 27 seconds-compared to over two minutes with the old kit. And survival rates jumped.
Here’s the bottom line: if you or someone you care for takes insulin, you need one of these ready-to-use glucagon products. Not the old kit. Not a backup. One that’s already ready to go. Keep it in your bag, your car, your child’s backpack. Check the expiration date every six months.
What About Severe Hyperglycemia?
High blood sugar isn’t just about feeling tired. When it climbs above 250 mg/dL and your body starts making ketones, you’re in danger of diabetic ketoacidosis (DKA). If it hits 600 mg/dL or higher with extreme dehydration, it’s hyperosmolar hyperglycemic state (HHS)-a silent killer.DKA often starts with nausea, fruity-smelling breath, and rapid breathing. HHS creeps up slowly-intense thirst, confusion, dry skin. Both can lead to coma or death if untreated. The mortality rate for untreated DKA? Up to 70%. With proper care? Under 5%.
Unlike hypoglycemia, you don’t treat this at home. You go to the ER. But you can prepare.

How Emergency Teams Handle Hyperglycemic Crises
In the hospital, doctors follow a strict three-step plan:- Fluids: They give 1-2 liters of IV saline in the first hour to rehydrate you. Dehydration is the biggest threat.
- Electrolytes: Potassium drops dangerously low during DKA. They replace it slowly through IV to protect your heart.
- Insulin: A continuous IV drip of regular insulin lowers blood sugar gradually. Never a bolus. Never rapid.
Important: You never give glucagon for high blood sugar. That’s like pouring gasoline on a fire. And you never give insulin without checking ketones first. A 2020 study found 12% of DKA patients developed dangerous low potassium levels because they got insulin too fast without proper monitoring.
Today, hospitals test blood ketones at the bedside. If your ketone level is above 1.5 mmol/L, it’s an emergency. Don’t wait. Call 911.
Why People Don’t Act-And What You Can Do
A 2022 survey found that 63% of people with type 1 diabetes have had a severe low. But only 41% always carry glucagon. Why? Fear. Confusion. They think they’ll mess it up.Here’s the truth: you won’t. The new nasal spray and autoinjector are designed for anyone-even a 12-year-old. Practice with a trainer device. Watch a 30-minute video from the American Diabetes Association. You’ll go from scared to confident.
And for hyperglycemia? People wait. They think, “I’ll just take an extra shot.” But without knowing ketone levels, that’s dangerous. If your blood sugar is over 250 mg/dL and you’re feeling sick, test for ketones. If they’re high, go to the ER. No excuses.

What Your Emergency Kit Should Contain
Build a simple kit. Keep it in one place-your purse, your fridge, your child’s school bag.- One ready-to-use glucagon (Baqsimi or Gvoke)-check expiration date
- Glucose tablets (15g total-four 4g tablets)
- Glucose gel or juice box (for mild lows, if conscious)
- Home ketone test strips and meter
- Emergency contact list: doctor, family, 911
- Medical ID bracelet
Never rely on someone else to know what to do. Write instructions on a card: “If unconscious, use nasal glucagon. Call 911. Do not give food or drink.”
New Tech Is Changing the Game
The first dual-hormone artificial pancreas, the Beta Bionics iLet, was approved in 2023. It automatically gives tiny doses of glucagon when it predicts a low. In trials, it cut severe hypoglycemia by 72%. But it’s only available at 12 U.S. centers right now.Meanwhile, apps like Gvoke HelperApp walk you through each step with video prompts. Glucagon prescriptions now often come with free training videos. Insurance coverage is improving-but 31% of Medicaid patients still face delays getting it approved.
And here’s the hard truth: Black and Hispanic patients are 2.3 times more likely to be hospitalized for severe lows. It’s not about biology. It’s about access. If you can get glucagon, make sure others can too.
Final Warning: Don’t Guess. Test.
If you’re unsure whether someone is having a low or a high, check the blood sugar. If you can’t test, assume it’s low. Glucagon won’t hurt someone with high blood sugar-it just won’t work. But giving insulin to someone who’s low? That’s fatal.Emergency care for diabetes isn’t about fancy machines or complicated protocols. It’s about having the right tool, knowing how to use it, and acting fast. Your life-or someone else’s-could depend on it.
What should I do if someone with diabetes is unconscious and I don’t have glucagon?
Call 911 immediately. Do not try to give them food, drink, or insulin. If they’re unconscious, putting anything in their mouth risks choking. Emergency responders have IV glucose and can treat them safely. Keep your phone charged and your emergency contacts handy.
Can I use glucagon for high blood sugar?
No. Glucagon raises blood sugar. Giving it during hyperglycemia can make DKA or HHS worse. Only use glucagon when blood sugar is confirmed below 54 mg/dL and the person can’t treat themselves. If you’re unsure, check the glucose level first. If you can’t test, assume it’s low and use glucagon-it’s safer than doing nothing.
Why do I need to test for ketones when my blood sugar is high?
High blood sugar alone isn’t always an emergency. But if your body starts breaking down fat for energy, it produces ketones. Levels above 1.5 mmol/L mean you’re at risk for diabetic ketoacidosis (DKA). Ketones are silent killers-they can cause coma without obvious symptoms. Always test if your sugar is over 250 mg/dL and you feel nauseous, breathless, or confused.
Are the new glucagon products covered by insurance?
Most private insurance plans cover Baqsimi and Gvoke, but coverage varies. Medicaid coverage is patchier-31% of patients face prior authorization delays. Talk to your pharmacist or diabetes educator. Some manufacturers offer copay cards or free samples. Never wait until an emergency to get it. Get your prescription now, even if you’ve never had a severe low.
How often should I practice using glucagon?
Practice every three months using a trainer device (most kits come with one). Studies show people who practice retain 92% of their skills after six months. Without practice, skills drop to 45%. Practice on a family member or friend. Make it routine-like checking your blood sugar. Confidence saves lives.
Can type 2 diabetes patients on insulin also need glucagon?
Yes. Anyone taking insulin-whether type 1 or type 2-is at risk for severe hypoglycemia. Yet only 34% of type 2 patients on insulin carry glucagon, compared to 68% of type 1 patients. Risk isn’t about diabetes type-it’s about medication. If insulin is part of your treatment, you need glucagon. Period.





Write a comment
Your email address will be restricted to us