When you walk into a doctor’s office and hear your blood pressure reading-120/80-it’s easy to think that’s the golden standard for everyone. But what if that number isn’t right for you? The truth is, there’s a growing divide in how doctors approach blood pressure targets. Some say everyone should aim for 120/80. Others argue that’s too aggressive, especially for older adults or those with other health issues. So who’s right? And what should you actually be targeting?
Why 120/80 Became the New Normal
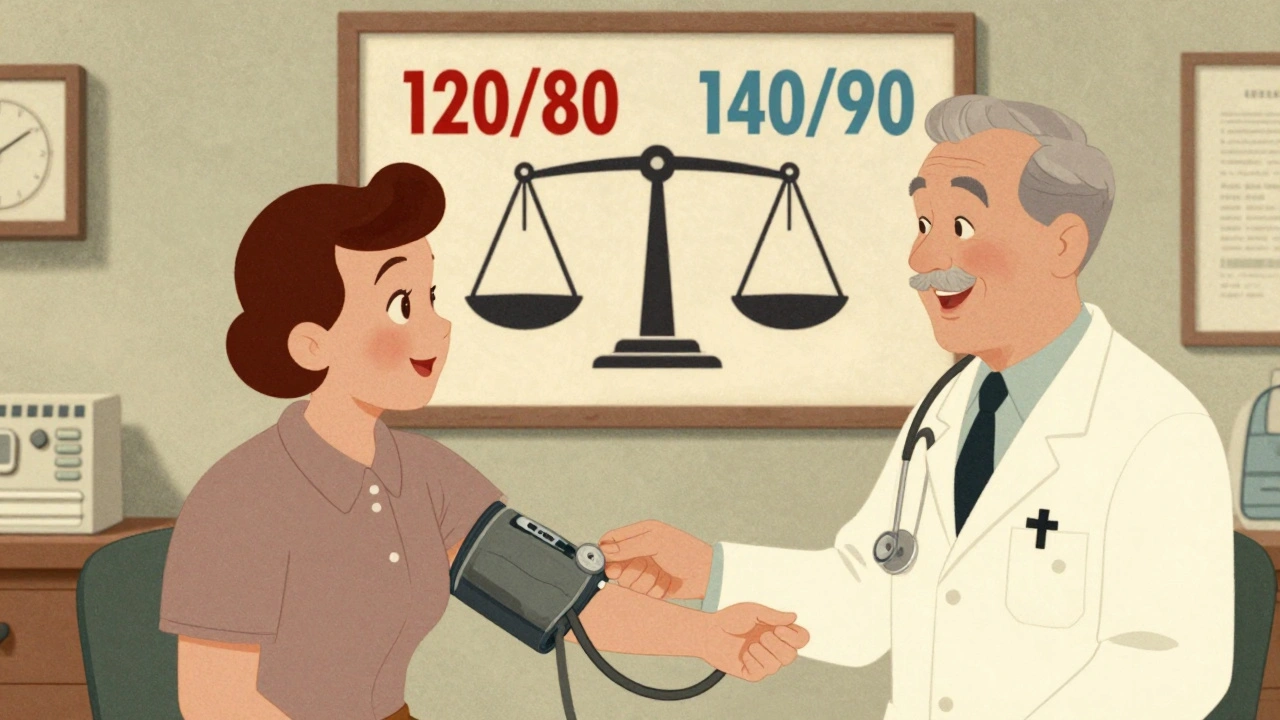
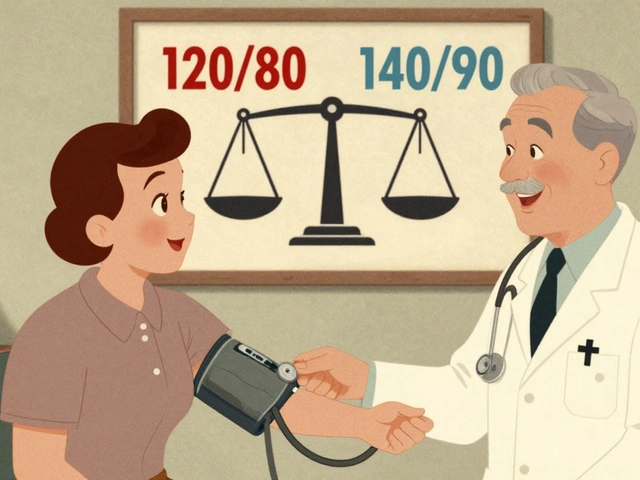
The push for a lower target-120 mm Hg systolic and 80 mm Hg diastolic-came from the SPRINT trial in 2015. This major study followed over 9,300 adults with high blood pressure but no diabetes or stroke history. Those who were treated to get their systolic pressure below 120 had 25% fewer heart attacks, strokes, and heart failure events. Mortality dropped by 27%. It was a big deal. And it led the American Heart Association and American College of Cardiology to update their 2017 guidelines, lowering the definition of high blood pressure from 140/90 to 130/80. By 2025, those guidelines were reinforced. The AHA/ACC now recommends aiming for under 130 mm Hg systolic for most adults with hypertension. If you’re healthy enough and your doctor thinks you can handle it, they’ll push for under 120. The logic is simple: every 5 mm Hg drop in systolic pressure cuts your risk of major heart events by about 10%. That’s not small change. It’s life-saving.The Counterargument: Why 140/90 Still Makes Sense
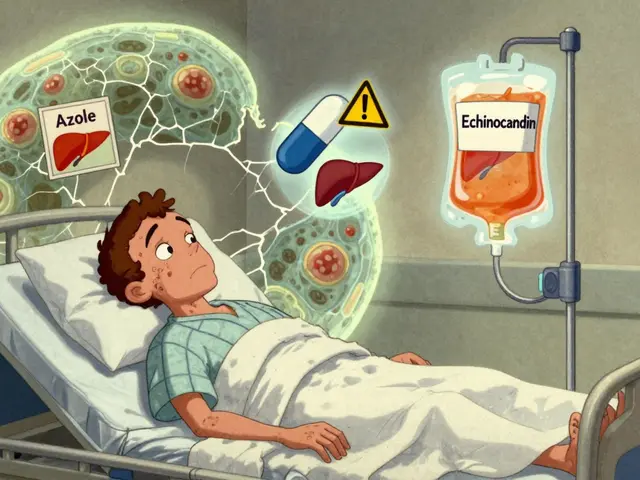
But here’s the catch. Not everyone in the SPRINT trial looked like you. The study excluded people over 75 with frailty, those with diabetes, and anyone at high risk of falling. Real-world patients? They’re different. Many are older. Many take multiple medications. Many have kidney problems or low blood pressure when they stand up. The American Academy of Family Physicians (AAFP) looked at the same data-and came to a different conclusion. In their 2022 review, they found that pushing systolic pressure below 130 didn’t reduce deaths. It didn’t even cut heart attacks much. The number needed to treat (NNT) to prevent one heart attack was 137 over 3.7 years. Meanwhile, the number needed to harm (NNH)-the number of people who’d have side effects like dizziness, fainting, or kidney trouble-was just 33. That’s a lot of people feeling worse just to help a few. They recommend sticking with 140/90 as the primary target. Not because it’s ideal, but because it’s safer for most people in primary care. And they’re not alone. The European Society of Hypertension takes a middle path: under 129/79 for people under 65, under 139 for those 65-79, and under 150 for those over 80. Age matters. Health matters. Life matters.What About Japan’s Bold Move?
In January 2025, Japan’s hypertension society dropped the ball on the old rules. Their new JSH2025 guidelines say: everyone-no exceptions-should aim for under 130/80. Even if you’re 85. Even if you’ve had falls before. Even if you’re on five meds already. Their reasoning? The Blood Pressure Lowering Treatment Trialists’ Collaboration, which analyzed data from over 400,000 people across 40 countries, showed that lowering systolic pressure by 5 mm Hg reduced heart events by 10% in every age group, every risk level, every background. Japan’s approach is aggressive. But they’ve built it on a system that makes it work: frequent monitoring, fast adjustments, and strong patient education. If you’re dizzy after a pill, you call your clinic. If your creatinine spikes, you get a blood test the same day. It’s not just about the number-it’s about how you get there.
Who Should Aim for 120/80?
If you’re under 65, have no major health problems, and your blood pressure is consistently above 130/80, then yes-120/80 is a reasonable goal. Especially if you have:- Diabetes
- Chronic kidney disease
- High 10-year cardiovascular risk (over 7.5%, calculated using tools like PREVENT)
- Already had a heart attack or stroke
Who Should Stick with 140/90?
If you’re over 75, especially if you’re frail, have memory issues, or have fallen before, 140/90 is safer. If you’re on multiple medications and already feel lightheaded standing up, pushing lower might do more harm than good. If your blood pressure drops too far, you risk:- Syncope (fainting)
- Acute kidney injury
- Electrolyte imbalances like high potassium
- Reduced quality of life
The Real Issue: It’s Not About the Number
The biggest mistake doctors and patients make is treating blood pressure like a score on a video game. Lower is always better. But it’s not. It’s about balance. It’s about what happens when you get there. A 78-year-old woman with mild dementia and a history of falls might have a BP of 145/85. If you push her to 125, she might fall, break her hip, end up in a nursing home. That’s not progress. That’s harm. A 52-year-old man with type 2 diabetes and a 12% risk of heart disease in 10 years? His BP should be 120/70. Not because he’s perfect, but because his body can handle it-and his future depends on it. That’s why shared decision-making isn’t just a buzzword. It’s the only way this works. Your doctor shouldn’t tell you your target. You should decide together-based on your health, your lifestyle, your fears, your goals.What You Can Do Right Now
You don’t need to wait for your next appointment to take control:- Get a home monitor. Check your BP twice a day, at the same times, for a week. Write it down.
- Know your numbers. Not just the reading, but what your doctor says they mean.
- Ask: “Is my goal based on my health, or just a number?”
- Ask: “What side effects should I watch for if we lower this?”
- Ask: “What happens if I don’t change anything?”
The Future: Personalized Blood Pressure
The next big shift won’t be in guidelines. It’ll be in tools. The NIH just launched SPRINT-2-a new trial with over 8,500 people, including those with diabetes and fall risk. It’s designed to answer the real-world question: Can we safely push lower targets for everyone? Meanwhile, researchers are building algorithms that combine genetics, kidney function, sleep patterns, and even social factors like loneliness to predict who will benefit from tight control-and who won’t. In five years, your BP target might not come from a guideline. It might come from your digital health profile. For now, though, the answer is simple: 120/80 is great-for some. 140/90 is fine-for others. The best target is the one that keeps you alive, well, and moving-without making you feel worse.Is 120/80 the right blood pressure target for everyone?
No. While 120/80 is ideal for younger, healthier adults-especially those with diabetes, kidney disease, or high heart disease risk-it’s not safe or necessary for everyone. For older adults, especially those over 75 or with frailty, a target of 140/90 is often safer and just as effective at preventing death and disability.
Why do some doctors want me to aim for 120/80 while others say 140/90 is fine?
It comes down to different interpretations of the same data. The American Heart Association and American College of Cardiology rely heavily on the SPRINT trial, which showed major benefits from lower targets. But the American Academy of Family Physicians looks at real-world outcomes and sees more side effects-like fainting and kidney issues-without clear gains in survival. One group focuses on what’s possible in ideal conditions; the other focuses on what’s safe in everyday practice.
Can I lower my blood pressure without medication?
Yes. Lifestyle changes can drop your systolic pressure by 10-15 mm Hg. Walk daily, reduce salt intake, lose even 5% of your body weight, limit alcohol, and manage stress. These steps work for most people and often reduce or delay the need for pills. They’re the foundation of any blood pressure plan.
What are the dangers of pushing blood pressure too low?
Too-low blood pressure can cause dizziness, fainting, falls, and injuries-especially in older adults. It can also harm your kidneys by reducing blood flow, raise potassium levels, and lead to dehydration from diuretics. In some cases, it increases the risk of cognitive decline because the brain isn’t getting enough steady blood flow.
How do I know if my blood pressure goal is right for me?
Ask your doctor: What’s my 10-year heart disease risk? Do I have diabetes or kidney disease? Have I had falls or dizziness? Am I on multiple medications? Your goal should match your health-not a guideline. If your doctor doesn’t ask these questions, it’s time to have a deeper conversation.


Write a comment
Your email address will be restricted to us