Drug Holiday Eligibility Checker
Check Your Eligibility
This tool helps you assess if you might qualify for a supervised drug holiday based on clinical guidelines. Always consult your doctor before making changes to medication.
Stopping your medication might sound like a bad idea - and often, it is. But what if taking a short, planned break from your prescription could actually help you feel better? This isn’t about skipping pills because you forgot or felt better. This is about drug holidays: carefully planned, doctor-supervised pauses in treatment designed to reduce side effects, reset your body’s response, or improve quality of life. It’s not for everyone. But for some people, it’s the difference between managing a condition and truly living with it.
What Exactly Is a Drug Holiday?
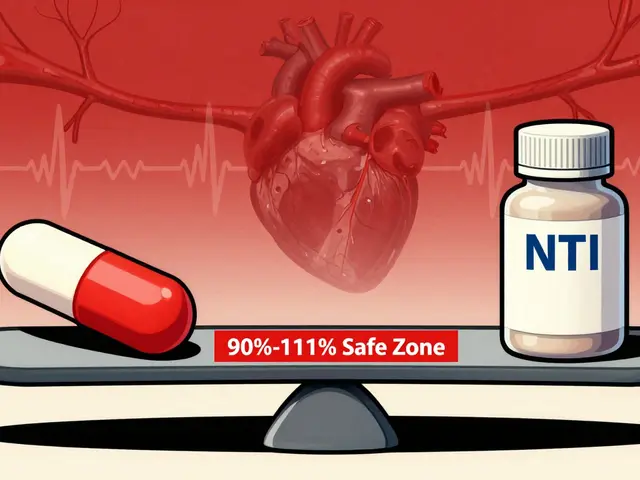
A drug holiday isn’t quitting your meds cold turkey. It’s a temporary, controlled stop - usually lasting days to weeks - done under medical supervision. The goal isn’t to cure anything. It’s to give your body a break from the constant presence of a drug so it can recover from unwanted side effects or reset how it responds to the medication. This approach started gaining attention in the 1990s with HIV treatment. Doctors thought interrupting antivirals might help the immune system recover. But by 2006, the SMART trial - involving over 5,000 people across 33 countries - proved the opposite. Interrupting HIV meds led to more infections, heart problems, and even deaths. Since then, the medical world has become much more cautious. Today, drug holidays are only considered in specific cases where the benefits clearly outweigh the risks.Where Drug Holidays Actually Work
Not all medications are created equal when it comes to taking breaks. Some can handle short pauses. Others can’t. The biggest factor? Half-life - how long the drug stays active in your body. Antidepressants (especially SSRIs) are one of the most common candidates. Medications like fluoxetine (Prozac) have a long half-life - around 4 to 6 days. That means even if you skip a couple of doses, the drug is still in your system. This makes short weekend breaks (48-72 hours) possible without triggering withdrawal symptoms like dizziness, nausea, or “brain zaps.” Studies show about 65% of people on SSRIs report improved sexual function after these short breaks, with no increase in depression symptoms. For someone struggling with loss of libido or delayed orgasm, that’s a major quality-of-life win. ADHD medications like methylphenidate (Ritalin) or amphetamine (Adderall) are another area where drug holidays are tried - mostly in kids. Parents often pause meds during summer break or holidays, hoping to avoid side effects like appetite loss or slowed growth. But here’s the catch: 78% of children experience a sharp rebound in symptoms. That means more impulsivity, emotional outbursts, trouble sleeping, and even accidents. One mother told the Child Mind Institute her son went from being a happy camper to ending up in the ER three times during a summer without meds. The American Academy of Child and Adolescent Psychiatry says these breaks can help with growth in 15-20% of cases, but they increase the risk of accidents by 45%. That’s not a trade-off most families can afford.The Dangerous Side of Skipping Pills
Some medications are absolutely not safe to stop suddenly. Stopping beta-blockers can trigger heart attacks. Stopping seizure meds can cause life-threatening seizures. Stopping steroids can lead to adrenal crisis - a sudden drop in cortisol that can kill you if not treated fast. Even for drugs where breaks are possible, unsupervised stopping is dangerous. A 2023 survey on Drugs.com found 41% of people who took unplanned antidepressant breaks experienced withdrawal symptoms like brain zaps, vertigo, or flu-like feelings. These aren’t just uncomfortable - they can make someone think their depression is coming back, when it’s really just their body reacting to the absence of the drug. And here’s something most people don’t realize: stopping meds without guidance often leads to longer-term problems. People who quit cold turkey are more likely to stop taking their meds altogether - even if they need them. The CDC says 61% of emergency visits related to psychiatric meds involve people who stopped on their own.
Who Should Consider a Drug Holiday?
Not everyone qualifies. You need to meet certain criteria:- Your condition has been stable for at least 6 months.
- You’re on a medication with a long half-life (like fluoxetine, not paroxetine).
- You’re experiencing a specific, measurable side effect - like sexual dysfunction, weight gain, or insomnia - that’s affecting your daily life.
- You have a support system: family, caregivers, or a therapist who can watch for warning signs.
- You’ve discussed it with your doctor and have a written plan.
How to Do It Right
If your doctor agrees a drug holiday might help, here’s how to make it safe:- Track your symptoms first. For 4-8 weeks, log your mood, sleep, energy, side effects, and daily functioning. This gives your doctor a baseline.
- Set clear rules. How long will the break last? What signs mean you must restart? (e.g., “If I feel hopeless for two days straight, I go back on meds.”)
- Use gradual steps if needed. For some, cutting the dose by 25% per week before stopping helps avoid withdrawal.
- Plan for the return. Know exactly when and how you’ll restart. Don’t wait until you’re in crisis.
- Get a follow-up. Most guidelines recommend a check-in within 72 hours after restarting.

Real Stories: The Good, the Bad, and the Ugly
On Reddit’s r/ADHD community, 62% of parents who tried summer breaks said it made family life worse. One parent wrote: “My 10-year-old couldn’t sit still at the pool. He ran into traffic. We spent two weeks in crisis mode.” But on PatientsLikeMe, 78% of people on weekend SSRI breaks said their relationships improved. “Two days off Prozac brought back intimacy,” wrote one user. “No mood swings. No anxiety. Just us again.” The difference? One group had no plan. The other had structure.The Future of Drug Holidays
The field is changing fast. In 2023, the FDA approved a new extended-release version of bupropion designed with built-in “holiday windows” - timed pauses to reduce sexual side effects without full discontinuation. Meanwhile, the NIH’s SPRINT trial is testing whether genetic testing can predict who’s safe to take a break. Early results suggest some people’s DNA makes them more resistant to withdrawal. AI tools are also being developed to predict relapse risk. One model in development can analyze your medication history, symptom patterns, and even sleep data to tell you if a break is likely to backfire. These won’t replace doctors - but they’ll help them make smarter calls.Bottom Line: It’s Not About Skipping Pills - It’s About Smart Management
Drug holidays aren’t a shortcut. They’re not a way to avoid taking your meds forever. They’re a tool - used carefully, with expert guidance - to make treatment more tolerable. If you’re struggling with side effects, don’t assume you’re stuck. Talk to your doctor. Bring your symptom log. Ask: “Could a short, planned break help?” But never do it alone. The risks of unsupervised stopping are real. And the relief you might feel from a weekend off? It’s only worth it if you can come back safely.Are drug holidays safe for everyone?
No. Drug holidays are only safe for certain medications and under medical supervision. They’re not safe for blood pressure drugs, seizure medications, or steroids. Even for antidepressants or ADHD meds, they carry risks if not planned properly. Always talk to your doctor before stopping any prescription.
Can I take a drug holiday if I feel better?
Feeling better doesn’t mean you don’t need the medication. Many psychiatric and neurological conditions require ongoing treatment to stay stable. Stopping because you feel fine is one of the most common reasons people relapse. Only consider a break if your doctor agrees it’s appropriate for your specific situation.
How long should a drug holiday last?
It depends on the drug. For SSRIs like fluoxetine, 48-72 hours is common for side effect relief. For ADHD meds in children, breaks may last 6-12 weeks during summer - but only with close monitoring. Never extend a break beyond your doctor’s plan.
What are the signs I should restart my medication?
Watch for return of original symptoms: mood swings, irritability, trouble focusing, sleep problems, or anxiety. For ADHD, watch for impulsivity, accidents, or social withdrawal. For depression, watch for hopelessness, loss of interest, or fatigue. If any of these appear, restart your medication immediately and contact your doctor.
Can I do a drug holiday without telling my doctor?
No. Unsupervised medication breaks are dangerous and are linked to 61% of emergency visits related to psychiatric drugs. Withdrawal symptoms can be mistaken for relapse, leading to incorrect treatment decisions. Always work with your provider - even if you think you know what you’re doing.






Write a comment
Your email address will be restricted to us