Targeted Therapy Matchmaker
EGFR: Found in lung cancer; targeted by drugs like erlotinib.
HER2: Present in some breast cancers; treated with trastuzumab.
BRAF: Mutated in melanoma; targeted by vemurafenib.
BRCA: Defective in ovarian and breast cancers; treated with PARP inhibitors.
Targeted drugs act like keys that fit specific locks (biomarkers) on cancer cells. They block specific molecular pathways that drive cancer growth.
Unlike chemotherapy, they typically cause fewer side effects because they don't harm healthy cells.
While targeted therapy generally causes fewer side effects than chemotherapy, common ones include:
- Skin rash or dryness
- Diarrhea
- Hypertension
- Liver enzyme elevations
Most side effects can be managed with dose adjustments or supportive care.
Quick Takeaways
- Targeted therapy attacks cancer cells by zeroing in on specific molecular abnormalities.
- It often works better and with fewer side effects than traditional chemotherapy.
- Key biomarkers such as EGFR, HER2, and BRAF determine which patients benefit.
- Several major cancers-including lung, breast, and melanoma-already have FDA‑approved targeted drugs.
- The next wave will combine targeted agents with immunotherapy and AI‑driven diagnostics.
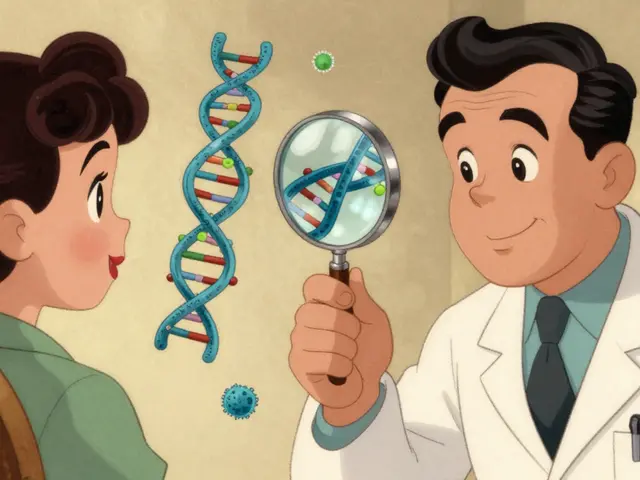
What Exactly Is Targeted Therapy?
Targeted therapy is a treatment approach that uses drugs or other substances to precisely attack cancer cells based on specific molecular targets. Unlike chemotherapy, which attacks any rapidly dividing cell, targeted drugs latch onto proteins or genes that are unique to the tumor. This precision means doctors can often give a lower dose, reducing collateral damage to healthy tissue.
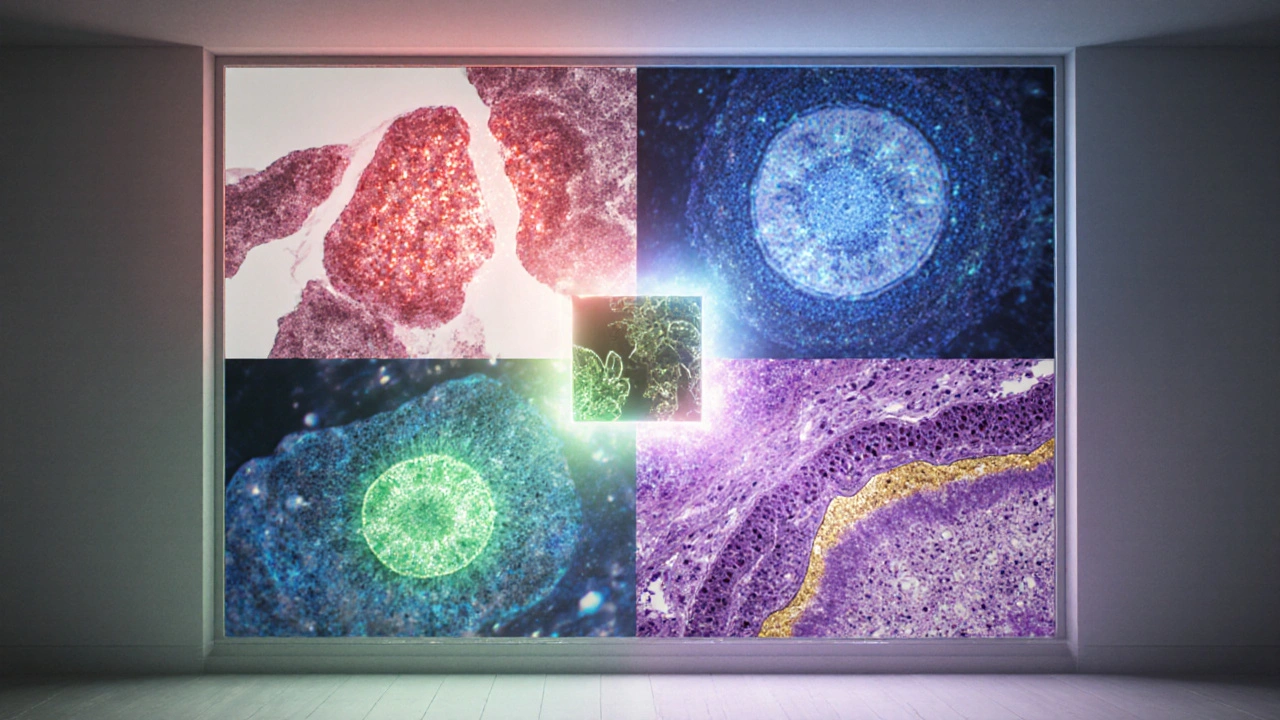
How Does It Work? Molecular Targets and Biomarkers
At the heart of targeted therapy are biomarkers measurable DNA, RNA, or protein signatures that indicate a tumor’s vulnerability. A test-often a tissue biopsy or a liquid biopsy-detects a mutation like an EGFR alteration in non‑small cell lung cancer. Once identified, a drug that specifically blocks that mutant protein can be prescribed.
Think of a lock (the biomarker) and a key (the drug). When the key fits, the lock jams the cancer’s growth engine. This lock‑and‑key model is why a single drug can be wildly effective in one patient but useless in another.
Key Cancer Types That Benefit Today
Over the past decade, the FDA has approved more than 70 targeted agents. Here are the biggest winners:
- Lung cancer: EGFR inhibitors (e.g., erlotinib) and ALK inhibitors (e.g., alectinib) have turned once‑terminal diagnoses into chronic conditions for many patients.
- Breast cancer: HER2‑positive tumors respond dramatically to trastuzumab and newer agents like pertuzumab.
- Melanoma: BRAF inhibitors (vemurafenib, dabrafenib) plus MEK inhibitors keep tumor growth in check for a large subset of patients.
- Ovarian and breast cancers with BRCA mutations: PARP inhibitors (olaparib) exploit DNA repair weaknesses.
- Colorectal cancer: Anti‑VEGF drugs (bevacizumab) and KRAS‑wildtype therapies extend survival.
Each of these examples illustrates the core principle: match the drug to the tumor’s genetic profile.
Benefits Over Traditional Chemotherapy
| Aspect | Targeted Therapy | Chemotherapy | Immunotherapy |
|---|---|---|---|
| Mechanism | Blocks specific molecular pathways | Damages rapidly dividing cells | Activates the immune system |
| Side‑Effect Profile | Generally milder; skin rash, diarrhea | Severe; nausea, hair loss, marrow suppression | Immune‑related inflammation, endocrinopathies |
| Response Predictability | High when biomarker present | Variable, often non‑specific | Dependent on tumor mutational burden |
| Typical Treatment Duration | Months to years (continuous dosing) | Cycles of weeks | Cycles or continuous depending on regimen |
The table shows why many oncologists now start with a targeted agent if a relevant biomarker is found. It’s not a blanket replacement for chemo, but it often reduces the number of chemo cycles a patient needs.
Side Effects and How to Manage Them
Even though targeted drugs spare healthy cells, they’re not completely harmless. Common toxicities include skin rash, hypertension, and liver enzyme elevation. Physicians usually monitor labs every 2-4 weeks during the first few months.
When a side effect spikes, the typical approach is dose interruption followed by a reduced dose. For example, a patient on a VEGF inhibitor who develops high blood pressure might receive antihypertensive medication and have the cancer drug paused until the pressure normalizes.
Current Landscape: FDA Approvals and Clinical Trials
The FDA U.S. Food and Drug Administration, the agency that reviews and authorizes new medical treatments approves a new targeted agent roughly every six months. Many of these approvals stem from clinical trials research studies that test safety and efficacy of new therapies in patients that use adaptive designs to speed up enrollment.
If you’re considering a new drug, ask your oncologist about ongoing trials. Platforms like ClinicalTrials.gov list studies by cancer type, mutation, and location, making it easier to find a match.
Future Trends: Combination Strategies and AI‑Driven Matching
Scientists are now exploring combos that pair a targeted inhibitor with an immunotherapy treatment that helps the immune system recognize and kill cancer cells. Early data suggest that blocking a tumor’s growth pathway can make it more visible to immune cells.
Another frontier is AI‑based genomics. Algorithms sift through a patient’s entire DNA profile, flagging rare mutations that might respond to off‑label drugs. This could expand the pool of patients who benefit beyond the current 10‑15% of solid‑tumor cases.
Finally, the concept of "precision oncology" is evolving into "patient‑centred oncology," where lifestyle, comorbidities, and personal preferences shape the therapy mix. The goal isn’t just longer survival-it’s better quality of life.
Quick Checklist for Patients Considering Targeted Therapy
- Ask for molecular testing if you’re newly diagnosed.
- Verify that the identified biomarker has an FDA‑approved drug.
- Discuss potential side effects and monitoring schedule.
- Inquire about clinical trials that might offer newer agents.
- Consider insurance coverage; many plans now require prior authorization for targeted drugs.

Frequently Asked Questions
How is targeted therapy different from chemotherapy?
Targeted therapy aims at specific molecular changes in cancer cells, while chemotherapy attacks all fast‑growing cells. This selectivity often means fewer side effects and a higher chance of response when the right biomarker is present.
Do all cancers have a targetable mutation?
No. Currently, about 10‑15% of solid tumors have an FDA‑approved targeted option. Ongoing research is expanding that number, especially for rare mutations.
Can targeted therapy be used together with other treatments?
Yes. Many protocols combine targeted agents with chemotherapy, radiation, or immunotherapy to improve outcomes. However, combos can increase toxicity, so they must be managed carefully.
What are the most common side effects?
Side effects vary by drug but frequently include skin rash, diarrhea, hypertension, and liver enzyme changes. Most are reversible with dose adjustments or supportive medication.
How can I find out if I’m eligible for a targeted drug?
Ask your oncologist for comprehensive genomic profiling. The test results will list any actionable mutations and the corresponding FDA‑approved drugs or clinical trials.





Write a comment
Your email address will be restricted to us