When you pick up a generic pill at the pharmacy, you might wonder: is this really the same as the brand-name drug? After all, it looks different, costs a fraction of the price, and sometimes comes from a company you’ve never heard of. But here’s the truth: generic absorption rates aren’t just close to brand drugs-they’re tightly controlled to be clinically identical. The system isn’t perfect, but it’s built on decades of science, not guesswork.
What ‘Same Absorption’ Actually Means
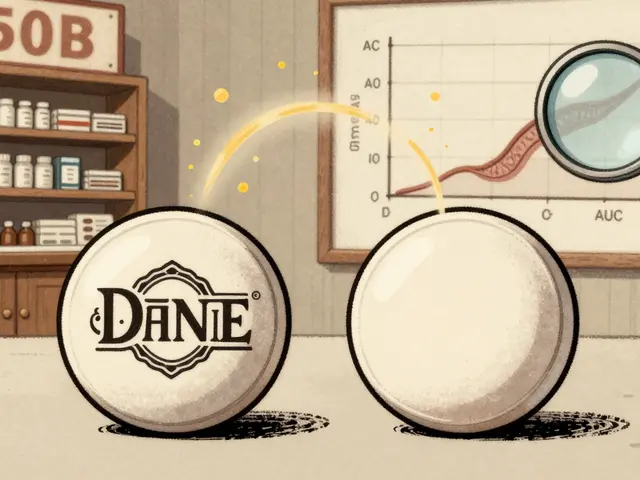
Generic drugs don’t need to be identical in appearance, taste, or filler ingredients. But they must deliver the same active ingredient into your bloodstream at the same rate and extent as the brand-name version. This is called bioequivalence. The U.S. Food and Drug Administration (FDA) sets the rules, and they’re strict. For a generic to be approved, the amount of drug your body absorbs-measured by two key numbers-must fall within 80% to 125% of the brand-name drug’s values.
Those two numbers are AUC and Cmax. AUC, or Area Under the Curve, tells you how much of the drug gets into your system over time. Cmax, or Maximum Concentration, shows how fast it gets there. Think of AUC as the total dose you receive, and Cmax as how quickly it hits its peak. Both must stay within that 80-125% range, and not just on average-every single study must show that the 90% confidence interval for both values fits entirely inside those bounds. That’s not a suggestion. It’s a legal requirement.
It’s easy to misread this. Some people think generics can be 20% weaker or 25% stronger. That’s wrong. The 80-125% range isn’t about how much the drug can vary-it’s about how tightly the testing must confirm similarity. In reality, the average difference between generics and brand drugs is only about 3.5%. For over 98% of approved generics, the absorption difference is less than 10%. That’s not just close. It’s nearly identical.
How Testing Works: Real People, Real Blood Samples
Generic manufacturers don’t just claim their drug works. They prove it. Every generic must pass an in vivo bioequivalence study. That means real people-usually 24 to 36 healthy volunteers-take both the brand-name drug and the generic version in a controlled setting. They’re given one, then after a washout period, the other. Blood samples are taken over hours to track how the drug moves through the body.
These aren’t lab simulations. They’re real human pharmacokinetics. The data from these studies is analyzed using geometric means, not simple averages, because drug absorption doesn’t follow a normal bell curve. The FDA requires that the 90% confidence interval for the ratio of geometric means (generic divided by brand) for both AUC and Cmax must lie entirely within 80-125%. If even one point of that interval crosses the line, the generic is rejected.
Between 1996 and 2007, over 2,000 such studies were submitted to the FDA. The average Cmax ratio was 1.00 ± 0.06. The average AUC ratio was 1.00 ± 0.04. In plain terms: the generic drug’s absorption was almost exactly the same as the brand. And this isn’t rare. It’s the norm.
Why Some Generics Dissolve Differently-But Still Work
Here’s where confusion creeps in. Some generic drugs dissolve slower or faster in the lab than their brand counterparts. A 2014 study found that more than half of tested generics showed significantly different dissolution rates at 120 minutes. One generic nifedipine dissolved much slower. Another amoxicillin dissolved faster. Meloxicam batches from the same company varied between each other.
So why are these still approved? Because dissolution isn’t the same as absorption. A pill might dissolve quickly in a test tube but not absorb well in the gut. Or it might dissolve slowly but still release the drug at the right pace in the body. What matters isn’t how fast the pill breaks down in water-it’s how fast the active ingredient enters your bloodstream. That’s why the FDA requires in vivo testing. If the blood levels match, the pill’s physical behavior in a lab doesn’t matter.
Think of it like two cars with different engines. One might rev faster, but if both reach 60 mph in the same time and use the same amount of fuel, they’re functionally equivalent. The FDA doesn’t care how the drug gets there-only that it gets there the same way.

When Differences Actually Matter: Narrow Therapeutic Index Drugs
There are exceptions. For drugs with a narrow therapeutic index-where even a small change in blood level can cause harm or fail to work-tighter rules apply. These include warfarin, digoxin, phenytoin, and levothyroxine. For these, the FDA requires the 90% confidence interval to fall within 90-111%, not 80-125%. That’s a much smaller window.
That’s why some doctors hesitate to switch patients from brand to generic for these drugs. It’s not because generics are unsafe. It’s because even a 5% shift in blood concentration can be risky for someone on a delicate balance. For example, a slight drop in levothyroxine absorption could cause hypothyroid symptoms. A small rise in phenytoin could trigger seizures.
The FDA’s Orange Book rates generics with an ‘A’ for therapeutic equivalence or a ‘B’ if there’s a known bioequivalence issue. Only ‘A’ rated generics are automatically substituted by pharmacists in 49 U.S. states. If you’re on one of these sensitive drugs, ask your pharmacist if your generic is ‘A’ rated. If you’re stable on a brand, switching might not be worth the risk-even if the science says it’s safe.
What Patients Report vs. What Science Shows
Despite the data, patients still report differences. Online forums like Reddit and Inspire are full of stories: “My generic bupropion made me feel zoned out.” “My thyroid meds don’t work like they used to.” Drugs.com analyzed over 1,200 reviews and found 12% of users reported perceived differences, with levothyroxine and bupropion being the most common complaints.
But here’s the catch: a 2023 meta-analysis of 47 studies involving nearly 10,000 patients found no difference in outcomes between generic and brand-name cardiovascular drugs. The FDA has documented only 12 cases of possible therapeutic failure out of more than 14,000 approved generics between 2008 and 2023. That’s a 0.08% failure rate.
So why the disconnect? Sometimes it’s the placebo effect. A patient who believes generics are inferior may feel worse simply because they expect to. Sometimes it’s switching between different generic manufacturers. One batch of generic levothyroxine might come from Company A, the next from Company B-even though both are ‘A’ rated. That’s not a flaw in the system; it’s how the market works. But for sensitive patients, even that small shift can trigger symptoms.
Pharmacists should warn patients: your generic might look different next time. That’s normal. It doesn’t mean it’s weaker. It just means a different company made it.
The Bigger Picture: Why This System Works
Generics make up 90% of all prescriptions in the U.S. but only 23% of drug spending. In 2023, the generic drug market was worth $135.7 billion. Without bioequivalence standards, this system would collapse. Patients couldn’t trust the cheaper option. Pharmacies couldn’t substitute automatically. Insurance companies couldn’t save billions.
The FDA didn’t invent this standard out of thin air. It was built on decades of data and biological variability. Healthy people absorb the same drug differently from one dose to the next-by 10-15% on average. So the 80-125% range isn’t arbitrary. It’s designed to account for natural human variation while still ensuring safety.
Europe and Japan use similar standards. The European Medicines Agency uses the exact same 80-125% range. Japan tightens it slightly for some drugs, but the principle is the same: prove equivalence in people, not just in labs.
What You Should Do
If you’re on a routine medication-blood pressure, cholesterol, antibiotics, antidepressants-there’s no reason to avoid generics. The science is clear. They work the same.
If you’re on a narrow therapeutic index drug, stick with the same generic manufacturer if you can. If you’re switched and feel different, tell your doctor. Don’t assume it’s the drug. But don’t ignore it either. Keep a log: when did the change happen? What symptoms appeared? Did you switch manufacturers?
And if your pharmacist gives you a new generic that looks different? Ask: “Is this the same as my last one?” and “Is it rated ‘A’?” You’re not being difficult. You’re being informed.
The system isn’t flawless. But it’s one of the most rigorously tested, data-driven drug approval systems in the world. And for 99.9% of people, it works exactly as intended: saving money without sacrificing safety.
Are generic drugs as effective as brand-name drugs?
Yes, for the vast majority of medications. Generic drugs must meet strict FDA bioequivalence standards, proving they deliver the same amount of active ingredient into the bloodstream at the same rate as the brand-name version. Studies show the average difference in absorption is only about 3.5%, and over 98% of generics differ by less than 10%. The FDA approves generics only after testing in real human subjects.
Why do some people say generics don’t work for them?
Some patients report changes in how they feel after switching to a generic, especially with drugs like levothyroxine or bupropion. These reports are often due to switching between different generic manufacturers, placebo effects, or unrelated health changes. While rare, some individuals may be more sensitive to small variations. If you notice a change, track your symptoms and talk to your doctor-but don’t assume the generic is ineffective without evidence.
What’s the difference between A-rated and B-rated generics?
The FDA’s Orange Book rates generics as ‘A’ or ‘B’. ‘A’ means the drug is therapeutically equivalent to the brand and can be substituted automatically. ‘B’ means there are known bioequivalence concerns-such as inconsistent absorption-and substitution may not be recommended. If you’re on a critical medication, ask your pharmacist if your generic has an ‘A’ rating.
Why do generics look different from brand-name drugs?
U.S. trademark laws require generics to look different from brand-name drugs in color, shape, and size. This prevents confusion and protects the brand’s intellectual property. These visual differences have no effect on how the drug works. The active ingredient, dosage, and absorption rate are identical.
Should I avoid generics for thyroid or seizure medications?
For drugs with a narrow therapeutic index-like levothyroxine, phenytoin, or digoxin-small changes in blood levels can be risky. The FDA requires tighter bioequivalence standards (90-111%) for these, but even then, switching between different generic manufacturers can cause noticeable effects. If you’re stable on a brand or a specific generic, it’s often safer to stick with it. Always consult your doctor before switching.




Write a comment
Your email address will be restricted to us