Tamoxifen-SSRI Compatibility Tool
This tool helps you understand the interaction between tamoxifen and common SSRIs. Select an antidepressant to see if it's safe to take with tamoxifen and learn how it affects endoxifen levels.
Result
Select an antidepressant to see compatibility information.
When a woman is diagnosed with estrogen receptor-positive breast cancer, tamoxifen is often the first line of treatment. It’s been used for decades, works well, and is affordable. But here’s the catch: many of these women also struggle with depression during treatment. That’s where SSRIs come in - antidepressants like Lexapro, Zoloft, or Paxil. The problem? Some of these antidepressants might be quietly reducing tamoxifen’s effectiveness. And that’s not just theory. It’s a real, measurable interaction that’s sparked years of debate among doctors, researchers, and patients.
How Tamoxifen Actually Works
Tamoxifen isn’t active when you swallow it. Your liver has to turn it into something else - endoxifen - before it can block estrogen in breast tissue. Endoxifen is what actually fights the cancer. And here’s the key: about 40% of that conversion depends on one enzyme - CYP2D6. If that enzyme is slowed down, endoxifen levels drop. That’s not a small change. Studies show endoxifen concentrations below 5.97 ng/mL are linked to higher recurrence risk. But not everyone’s enzyme works the same. About 7-10% of white Europeans are poor metabolizers - their CYP2D6 barely works at all. Even among those who can metabolize it normally, certain drugs can shut the enzyme down.
Which SSRIs Are the Problem?
Not all SSRIs are created equal when it comes to CYP2D6. Think of it like a dimmer switch. Some SSRIs turn it way down. Others barely flicker.
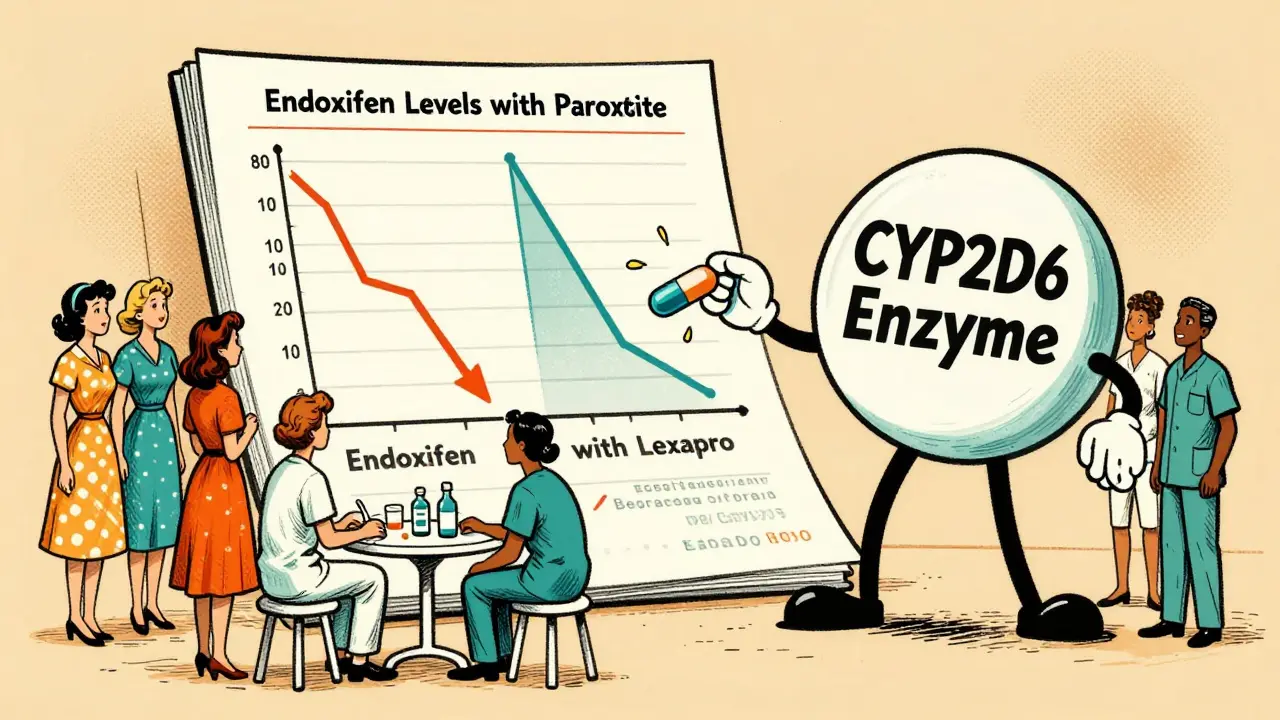
- Strong inhibitors: Paroxetine (Paxil) and fluoxetine (Prozac) - these are the worst offenders. One study showed paroxetine slashed endoxifen levels by over 60%.
- Moderate inhibitors: Sertraline (Zoloft) and venlafaxine (Effexor) - moderate drop, but not enough to trigger major concern in most studies.
- Weak inhibitors: Citalopram (Celexa) and escitalopram (Lexapro) - these barely touch CYP2D6. They’re the go-to alternatives for women on tamoxifen.
That’s why oncologists now avoid paroxetine like a landmine. In 2010, about 18% of tamoxifen users were on it. By 2022, that number dropped to 7%. The shift wasn’t random. It was driven by pharmacokinetic data and growing caution.
The Big Contradiction: Lab Results vs. Real-Life Outcomes
This is where things get messy. In the lab, the interaction is crystal clear. Give someone paroxetine with tamoxifen? Endoxifen crashes. But in real life? The results are all over the place.
A 2009 Canadian study followed 2,430 women and found those taking paroxetine had a 24% higher risk of dying from breast cancer. The risk jumped to 90% if they took it for more than six months. That scared a lot of doctors. But then came the Kaiser Permanente study in 2016 - 16,887 women, tracked for up to 14 years. No increased risk. Not even a hint. Same with a Danish study of over 16,000 women. No difference in recurrence. Even a 2023 Bayesian analysis found only a tiny increase in recurrence risk with CYP2D6 inhibitors - not enough to change practice.
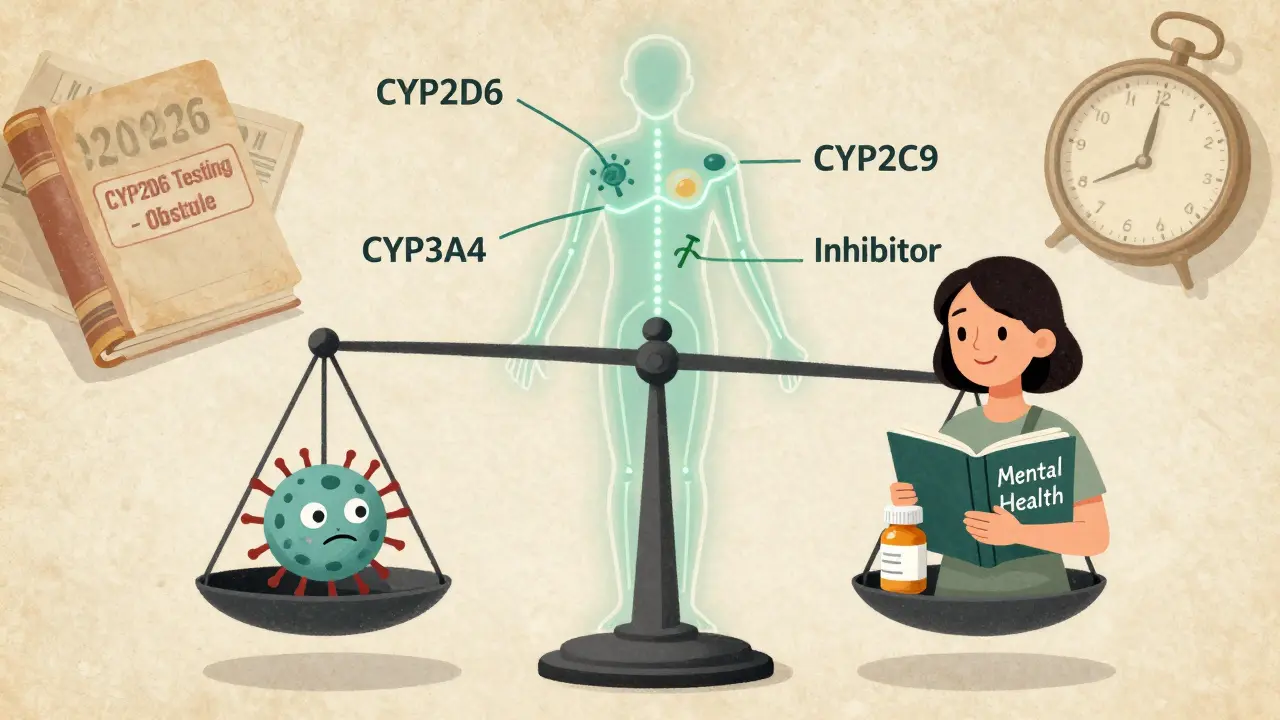
Why the split? Smaller studies didn’t account for things like cancer stage, age, or other meds. Bigger studies did. Timing matters too. Early recurrence might be affected, but long-term survival? Not so much. And here’s something important: tamoxifen doesn’t rely only on CYP2D6. Other enzymes like CYP3A4 and CYP2C9 can pick up the slack. Your body’s not a single-pathway machine.
What the Experts Really Say
Dr. Richard Kim, who led the 2009 Canadian study, still believes paroxetine should be off-limits. He says the data is too clear to ignore. But Dr. Nancy Davidson, former president of ASCO, says the opposite: ‘The totality of evidence does not support clinical concern.’
That’s why ASCO updated its guidelines in 2022 and said: Don’t avoid antidepressants because of CYP2D6. The FDA took a similar stance in 2012 - acknowledged the interaction, but said the data doesn’t prove it changes outcomes. The European Medicines Agency still warns against strong inhibitors, but even they’re starting to soften. The 2023 ESMO guidelines say the clinical relevance is ‘unproven.’
What’s changed isn’t the science - it’s the perspective. We used to think: if the drug level drops, the cancer comes back. Now we know: biology is more complex. The body adapts. Other pathways compensate. And the real driver of survival? Getting the right treatment, on time, and sticking with it - not just the exact concentration of one metabolite.
What Should You Do?
If you’re on tamoxifen and feeling depressed, don’t suffer in silence. Depression hurts your recovery more than any drug interaction. But choose wisely.
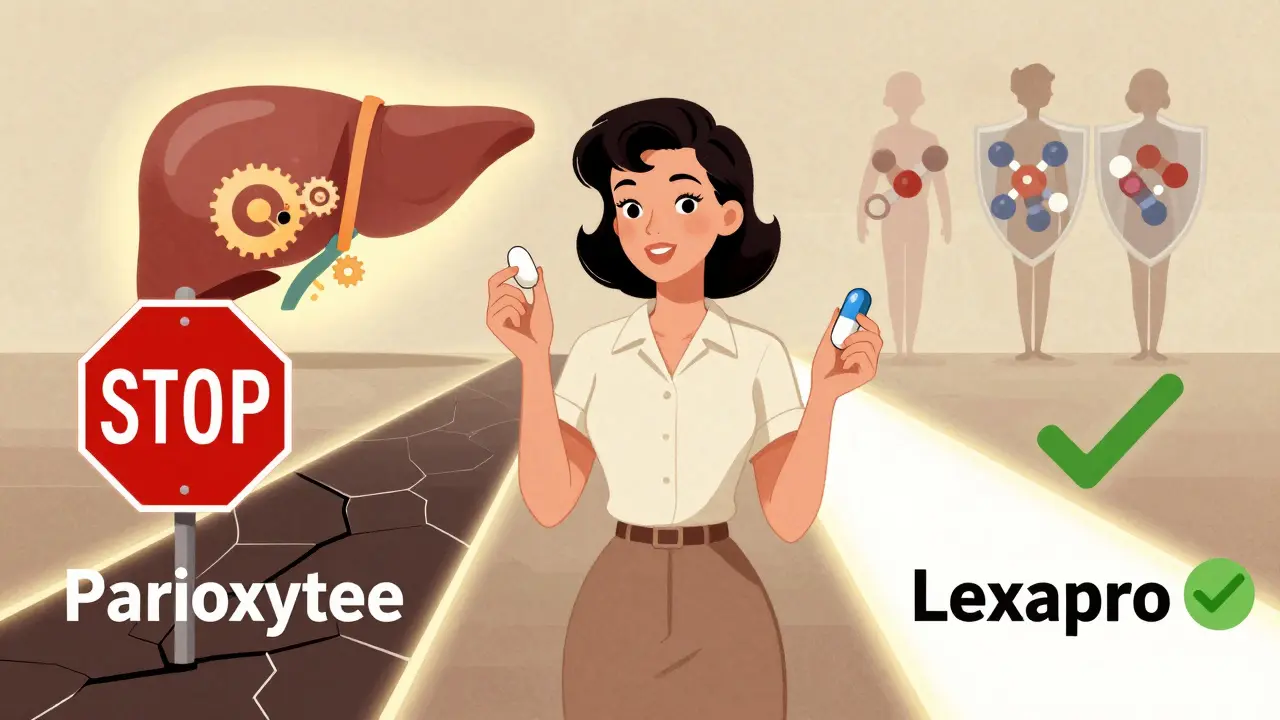
- Don’t take paroxetine or fluoxetine. Even if the risk is small, why risk it? These are the only two with consistent, strong evidence of interference.
- Choose escitalopram (Lexapro) or citalopram (Celexa). They’re effective for depression and don’t interfere with tamoxifen.
- Venlafaxine (Effexor) is also safe. It’s not an SSRI, but it’s a common alternative and has minimal CYP2D6 impact.
- Ask your doctor for the Flockhart Table. It’s a simple chart that ranks drugs by inhibition strength. Your oncologist should have it handy.
- Don’t stop your antidepressant without talking to your team. Switching meds can cause withdrawal or worsen depression. Do it slowly, under supervision.
Many hospitals now use electronic alerts in their systems. If you’re prescribed paroxetine while on tamoxifen, the computer flags it. In one study, that cut bad prescriptions by 37%. That’s not just tech - it’s better care.
The Future: Is Testing Even Worth It?
Years ago, some doctors pushed for CYP2D6 genetic testing before starting tamoxifen. The idea: if you’re a poor metabolizer, switch to an aromatase inhibitor. But that never panned out. Large studies showed no difference in outcomes between poor and normal metabolizers. The 2023 St. Gallen Consensus said testing isn’t useful. Dr. Veronique Michaud, who led a major 2023 analysis, predicts CYP2D6 testing for tamoxifen will be obsolete by 2026 - just like TPMT testing for chemotherapy.
The SWOG S1713 trial, expected to finish in 2025, will be the final word. It’s the first study to randomly assign women to either paroxetine or placebo while monitoring endoxifen levels. If endoxifen drops but cancer outcomes don’t change? That’s the nail in the coffin for the old theory.
Bottom Line
Yes, some SSRIs reduce endoxifen. Yes, that’s real. But no, that doesn’t mean your cancer will come back. The evidence doesn’t support it. What matters most is treating your depression - because untreated depression increases your risk of stopping tamoxifen, missing appointments, and dying from cancer. Don’t let fear of a drug interaction keep you from getting the mental health care you need.
Use escitalopram. Avoid paroxetine. Talk to your oncologist. And remember: your mental health is part of your cancer treatment. Not a side note. Not an afterthought. Essential.
Can I take Zoloft with tamoxifen?
Yes, sertraline (Zoloft) is considered a moderate CYP2D6 inhibitor. Studies show it reduces endoxifen levels by about 20-30%, but large outcome studies haven’t linked it to higher cancer recurrence. It’s not the first choice, but it’s safer than paroxetine or fluoxetine. If you’re already on Zoloft and doing well, don’t switch unless your doctor recommends it.
Is Lexapro safe with tamoxifen?
Yes, escitalopram (Lexapro) is one of the safest options. It’s a weak CYP2D6 inhibitor with almost no effect on endoxifen levels. It’s also well-tolerated and effective for depression. Most oncologists now recommend it as the first-line SSRI for women on tamoxifen.
What happens if I accidentally take Paxil with tamoxifen?
If you took paroxetine for a short time - a few days or weeks - don’t panic. The risk of harm is low. But don’t continue it. Talk to your doctor right away. They’ll likely switch you to escitalopram or citalopram. Long-term use (over 6 months) is where concern rises, but even then, outcome data is mixed. The priority is stopping the interaction, not stressing over what’s already happened.
Should I get tested for CYP2D6 before starting tamoxifen?
No. Major guidelines from ASCO, NCCN, and ESMO no longer recommend CYP2D6 testing. Studies show poor metabolizers don’t have worse outcomes than normal metabolizers. Testing adds cost, anxiety, and doesn’t change treatment. Focus on choosing the right antidepressant instead.
Are there other drugs that interfere with tamoxifen?
Yes. Besides SSRIs, other drugs like quinidine, bupropion (Wellbutrin), and some antifungals (like ketoconazole) can inhibit CYP2D6. Always tell your doctor and pharmacist you’re on tamoxifen before starting any new medication - even over-the-counter ones. Some cold medicines contain dextromethorphan, which can also interfere.
If you’re on tamoxifen and need help with depression, your mental health is just as important as your cancer treatment. There are safe, effective options. You don’t have to choose between feeling better and staying healthy. You can do both.


Write a comment
Your email address will be restricted to us