What is hypoparathyroidism?
When your parathyroid glands don’t make enough parathyroid hormone (PTH), your body can’t regulate calcium the way it should. This condition is called hypoparathyroidism. Without enough PTH, calcium levels in your blood drop too low, and phosphate builds up. You might feel tingling in your fingers, muscle cramps, or even seizures if it’s severe. Most cases happen after thyroid or neck surgery-about 8 out of 10 people who get this condition develop it after having their thyroid removed. But it can also come from autoimmune problems, genetic disorders like DiGeorge syndrome, or radiation damage to the neck.
Why calcium and vitamin D matter so much
PTH normally tells your bones to release calcium, your kidneys to hold onto calcium instead of peeing it out, and your gut to absorb more from food. When PTH is missing, all those signals stop. That’s why you need to replace what your body can’t make: calcium and active vitamin D. But here’s the catch-you don’t just take any vitamin D. Regular vitamin D3 (cholecalciferol) won’t work well because your kidneys can’t activate it without PTH. Instead, you need calcitriol or alfacalcidol-forms of vitamin D that are already activated. These bypass the broken step and get straight to work raising your calcium levels.
How much calcium should you take?
Most people start with 1,000 to 2,000 mg of calcium daily, split into two or three doses. But it’s not just about the total amount-it’s about timing and form. Calcium carbonate is the best choice because it’s 40% elemental calcium. That means you need less of it to get the same effect compared to calcium citrate, which is only 21%. For example, to get 1,000 mg of elemental calcium, you’d need about 2,500 mg of calcium carbonate. Take it with meals. That helps your body absorb it better and also acts as a phosphate binder, helping control high phosphate levels in your blood.
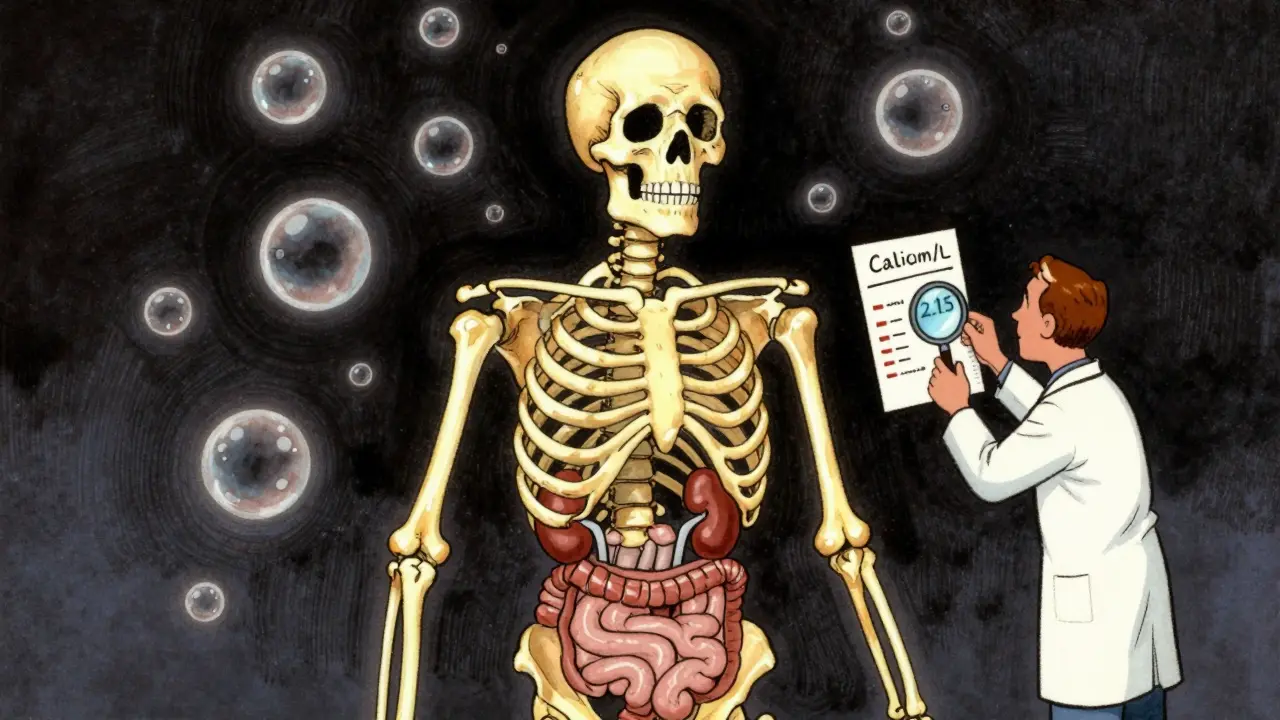
Active vitamin D dosing explained
Calcitriol is usually started at 0.25 to 0.5 micrograms per day. Some people need more, especially if they’ve had hypoparathyroidism for a long time. The goal isn’t to push calcium into the high normal range-it’s to keep it in the lower half of normal, around 2.00 to 2.25 mmol/L. Why? Because pushing calcium too high increases your risk of kidney stones, calcium deposits in your brain, and other long-term damage. One study found that people with calcium levels above 2.35 mmol/L for years had nearly three times the risk of brain calcification on MRI scans. That’s why doctors don’t aim for “normal” but for “safe.”
Why magnesium is often overlooked
If your magnesium is low, even the best calcium and vitamin D doses won’t work right. Magnesium helps your body respond to PTH and keeps your parathyroid glands functioning. Many people with hypoparathyroidism have low magnesium without knowing it. The target is 1.7 to 2.2 mg/dL. If you’re below that, you’ll need magnesium supplements-usually 400 to 800 mg of magnesium oxide or 200 to 400 mg of magnesium citrate daily. Without fixing this, your calcium levels will stay unstable no matter how many pills you take.
What to eat-and what to avoid
Food matters. You need calcium-rich foods: milk (300 mg per cup), yogurt, kale (100 mg per cup), broccoli (43 mg per cup), and fortified plant milks. But you also need to cut back on phosphate. Processed meats, hard cheeses, and soda are full of added phosphorus. A single liter of cola can have 500 mg of phosphoric acid. The goal is to keep daily phosphorus under 1,000 mg. That means reading labels and avoiding anything with “phos” in the ingredients. This isn’t just about feeling better-it’s about protecting your kidneys.
Monitoring: What your doctor checks
You won’t just get a blood test once a year. In the first few months, you’ll likely need blood work every 1 to 3 months. Your doctor will track:
- Serum calcium (target: 2.00-2.25 mmol/L)
- Serum phosphate (target: 2.5-4.5 mg/dL)
- Magnesium (target: 1.7-2.2 mg/dL)
- 24-hour urine calcium (target: under 250 mg/day)
High urine calcium means you’re at risk for kidney stones. If it’s over 250 mg/day, your doctor might lower your calcium dose, switch you to a thiazide diuretic like hydrochlorothiazide, or cut back on salt. Sodium makes your kidneys dump more calcium into urine, so keeping salt under 2,000 mg a day helps too.
When standard treatment isn’t enough
About 1 in 3 people with hypoparathyroidism struggle with conventional therapy. If you need more than 2 grams of calcium or more than 2 micrograms of calcitriol daily, or if you still get kidney stones or severe symptoms, it’s time to talk about alternatives. There’s a treatment called recombinant human PTH(1-84)-brand name Natpara. It’s a daily injection that replaces the missing hormone. Studies show it cuts calcium and vitamin D needs by 30-40%. But it’s expensive-around $15,000 a month-and hard to get because it requires special pharmacy handling and prior authorization. There’s also a new drug in development called TransCon PTH, which showed in a 2022 trial that it normalized calcium in 89% of patients with just one shot a day. It could be available soon.

Real-life challenges patients face
Managing this condition isn’t just about pills. One patient described it as a “calcium rollercoaster”-some days you feel fine, the next you’re tingling all over. Many take 6 to 10 pills a day. Constipation from calcium is common. Some people forget doses or run out because specialty pharmacies take 30 to 45 days to process refills. The Hypopara Alliance survey found that 68% of patients struggle to keep calcium stable. But small changes help: splitting calcium into four or five smaller doses a day, taking vitamin D at bedtime, and keeping magnesium up can make a big difference. One Cleveland Clinic study showed patients with magnesium above 1.9 mg/dL had 35% fewer symptoms.
What to do in an emergency
If you suddenly feel numb around your mouth, your hands cramp up, or you get a seizure, don’t wait. Chew 2 to 3 calcium tablets right away-each should give you 500 to 1,000 mg of elemental calcium. Then call your doctor or go to urgent care. Emergency IV calcium might be needed. Always carry a medical alert card or bracelet saying you have hypoparathyroidism. Many ER doctors have never seen a case.
What’s next for treatment?
Right now, we’re still using 1950s-era treatment for a 21st-century problem. But things are changing. Gene therapy targeting the calcium-sensing receptor is being tested in mice and could be ready for humans by 2026. The European Society of Endocrinology is updating its guidelines this year to better reflect long-term kidney risks. The goal isn’t just survival-it’s living without constant symptoms, without kidney damage, without fear of calcification in your brain or heart. Better tools are coming. Until then, the key is precision: the right dose, the right timing, and listening to your body.
Long-term outlook
Hypoparathyroidism is lifelong, but it doesn’t have to control your life. With careful management, most people live full, active lives. The biggest risks come from pushing calcium too high to feel better in the short term. The real win is stability-keeping calcium just low enough to protect your kidneys, but high enough to avoid numbness and cramps. It’s a tightrope walk, but with the right team and the right habits, you can stay balanced.