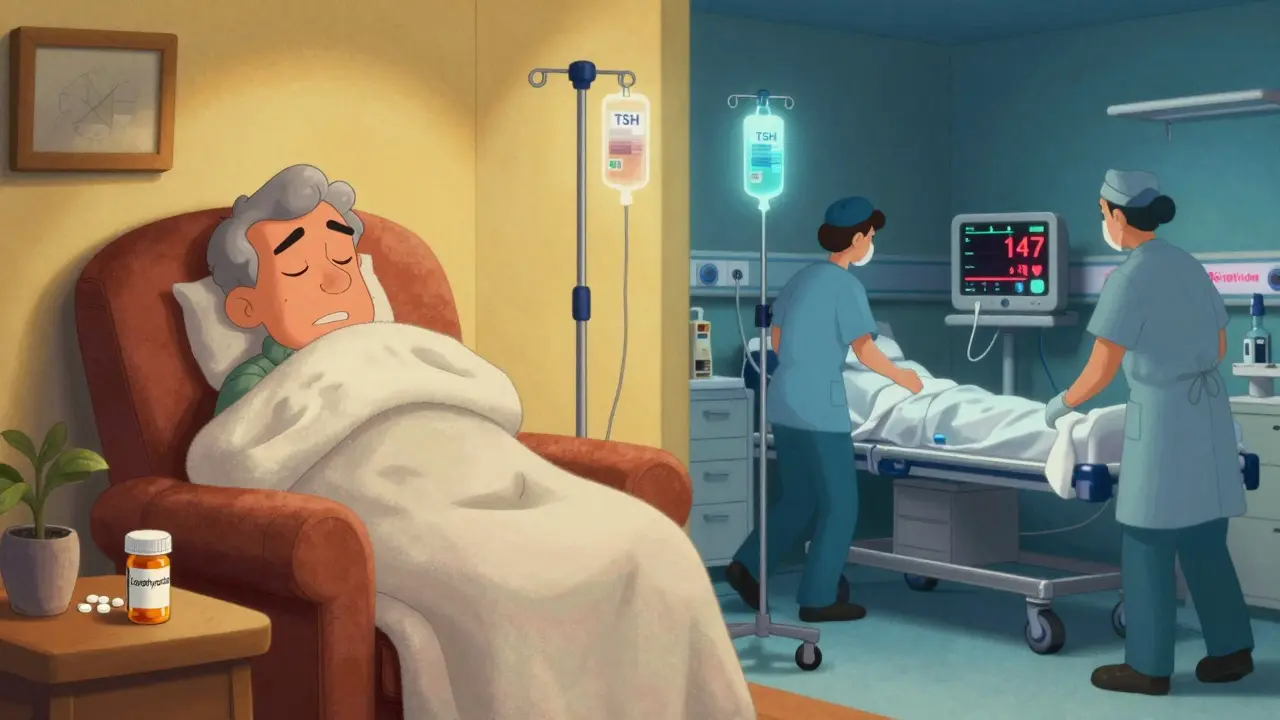
Myxedema coma isn't just a rare complication of hypothyroidism - it's a life-or-death emergency that kills 25% to 60% of people who don’t get help fast enough. You might think of it as "thyroid failure," but that’s not accurate. It’s the body shutting down because thyroid hormones have dropped so low that basic functions like breathing, heart rate, and temperature control stop working properly. And here’s the scary part: many patients aren’t diagnosed until they’re already unconscious. If you or someone you care about has long-standing hypothyroidism and suddenly starts acting confused, feeling freezing cold, or breathing too slowly, this could be it.
What Really Happens in Myxedema Coma?
Myxedema coma doesn’t come out of nowhere. It’s the final stage of untreated or poorly managed hypothyroidism, often after years of being on the wrong dose or not taking medication at all. The thyroid gland isn’t producing enough T3 and T4 - the hormones that tell your cells how fast to burn energy. Without them, your metabolism slows to a crawl. Your heart beats too slowly. Your lungs don’t push enough air. Your body can’t hold heat. And your brain? It starts to fog over, then shut down.
It’s not just about feeling tired. In myxedema coma, patients show a clear triad: altered mental status (confusion, drowsiness, coma), hypothermia (core temperature below 35°C or 95°F), and a precipitating event like infection, cold exposure, or stopping meds. Over 98% of cases involve extreme lethargy. Nearly 90% have dangerously low body temperature. And in 70-80% of cases, sodium levels crash below 135 mmol/L - a sign the body is in full survival mode.
Respiratory failure is common. Breathing drops below 12 breaths per minute. Carbon dioxide builds up. Oxygen levels plunge. Many patients need to be intubated just to keep breathing. Gastrointestinal problems follow - ileus (no gut movement), constipation, even megacolon. And because the kidneys slow down, fluid builds up, causing swelling in the face, eyelids, and legs - the classic "myxedema" swelling that gives the condition its name.
Who’s Most at Risk?
This isn’t a condition that hits young people often. About 75% of cases occur in women over 60. The female-to-male ratio is 3:1, but men are more likely to be misdiagnosed. Why? Because doctors often write off fatigue, cold sensitivity, or mental fog in older women as "just aging" or "depression." One patient on the American Thyroid Association’s forum said she was told she had depression for 18 months before she collapsed. Another man in his 50s, who had been on thyroid meds for years, stopped them during a hospital stay for pneumonia - and went into coma within days.
Winter is the deadliest season. Cold exposure is the #1 trigger. Even mild cold - like an unheated room or a drafty hospital ward - can push someone with borderline hypothyroidism into crisis. Infections are the next biggest trigger. Pneumonia, urinary tract infections, and even minor flu-like illnesses can be enough. A 2022 survey of 427 hypothyroid patients found that 47% of near-miss events happened during hospitalizations, and 32% followed infections.
And here’s the hidden gap: uninsured patients wait 35% longer for treatment and have 22% higher death rates. Delayed diagnosis isn’t just bad luck - it’s a systemic failure.
How Is It Different From Other Emergencies?
Think of endocrine emergencies as a family. Thyroid storm is the hyperactive cousin - too much hormone, racing heart, fever, agitation. Myxedema coma is its opposite: too little hormone, slow everything, freezing cold, unresponsive. Diabetic ketoacidosis has clear numbers: high blood sugar, low pH, low bicarbonate. Myxedema coma? There’s no single lab value that confirms it. TSH might be over 100 mIU/L. Free T4 might be below 0.9 ng/dL. But if you wait for those results, you might lose the patient.
Dr. Robert H. Eckel, former president of the American Heart Association, put it bluntly: "Myxedema coma represents one of the few true endocrine emergencies where treatment must not wait for laboratory confirmation." That’s why the top rule in emergency protocols is: start treatment before the lab report comes back.
Compare it to adrenal crisis - another deadly emergency. Both have high mortality. But adrenal crisis often comes with vomiting, abdominal pain, and low blood pressure. Myxedema coma? It looks like a slow-motion collapse. That’s why it’s missed.
The Emergency Protocol: What to Do
When you suspect myxedema coma, time isn’t just money - it’s life. The clock starts ticking from the moment symptoms appear. Every hour of delay increases the death risk by 10%. Here’s what needs to happen, in order:
- Secure the airway. Over half of patients need intubation because their breathing is too weak. Don’t wait for respiratory arrest. If they’re groggy and breathing under 12 times per minute, intubate.
- Give thyroid hormone immediately. The standard is a 300-500 mcg IV loading dose of levothyroxine (T4). In severe cases - especially with heart trouble - add 10-20 mcg of liothyronine (T3) every 8 hours. A 2022 Endocrine Society update found this combo cuts 30-day mortality by 15%.
- Warm the patient - gently. No heating blankets. No warm baths. Active rewarming can cause the heart to crash as the body demands more oxygen before the thyroid hormone kicks in. Use blankets, warm room, and monitor core temperature every 30 minutes. Passive rewarming only.
- Treat the trigger. If infection is suspected - and it usually is - start broad-spectrum antibiotics right away. Cover pneumonia and UTIs. Don’t wait for cultures. Infection is the cause in 30-50% of cases.
- Fix electrolytes slowly. Hyponatremia is common. But correcting sodium too fast can cause brain damage. Limit correction to 4-6 mmol/L in the first 24 hours. Use IV fluids with care - too much fluid worsens swelling and low sodium.
The DIMES mnemonic helps remember triggers: Drugs (like sedatives or opioids), Infection, Myocardial infarction or stroke, Exposure to cold, Stroke. Check for all five.
What Not to Do
Many mistakes are fatal.
- Don’t wait for labs. If the clinical picture fits, start treatment. Labs take hours. Death waits no time.
- Don’t use active warming. Heated blankets, warm IV fluids, or hot packs can trigger cardiac arrest.
- Don’t give glucose without steroids. If cortisol is low (common in severe hypothyroidism), giving glucose can cause a crash. Give hydrocortisone 100 mg IV before or with thyroid hormone.
- Don’t assume it’s dementia. Elderly patients often have "apathetic hypothyroidism" - no tremors, no swelling, no classic signs. Just confusion, low temperature, and slow heart rate. That’s myxedema coma.
Real Stories, Real Consequences
A 68-year-old woman in Manchester stopped her levothyroxine for three days while recovering from a cold. She started sleeping 20 hours a day, couldn’t stay warm even with three blankets, and became unresponsive. Her family thought she was depressed. By the time she got to the ER, her temperature was 32°C, her TSH was 147 mIU/L, and her sodium was 128 mmol/L. She spent 11 days in the ICU. She survived - but barely.
Another patient, a 72-year-old man with Hashimoto’s, was discharged from the hospital after a UTI with no thyroid check. Two days later, he was found in his kitchen, shivering, slurring words. He was dead on arrival. His wife said he’d been "just tired" for months. No one connected it.
These aren’t rare. A 2023 Lancet study found that 18% of hypothyroid patients had experienced a near-death event from missed or delayed care. Most were on medication - but didn’t get the right dose during stress.
The Future: Faster Detection, Better Outcomes
There’s hope. In January 2023, the FDA approved a new IV thyroid hormone called Thyrogen®, which works faster than older versions. Point-of-care thyroid tests are in phase 3 trials - they can give TSH and free T4 results in under 15 minutes. That could cut diagnosis time from hours to minutes.
Researchers are also tracking a new biomarker: thyrotropin receptor antibodies. A 2023 study showed these levels predict decompensation with 85% accuracy. In the next five years, we may be able to warn high-risk patients before they collapse.
But until then, the best tool is awareness. If you have hypothyroidism - or care for someone who does - know the signs. If they’re unusually sleepy, cold, slow, or confused - don’t wait. Call for help. Start the protocol. Because in myxedema coma, every minute counts.
Is myxedema coma the same as hypothyroidism?
No. Hypothyroidism is a chronic condition where the thyroid doesn’t make enough hormone - it’s common and manageable with daily medication. Myxedema coma is the extreme, life-threatening end of that spectrum, where the body shuts down due to critically low hormone levels. It’s not just worse hypothyroidism - it’s a medical emergency requiring immediate hospital care.
Can you survive myxedema coma?
Yes - but survival depends on how fast treatment starts. If thyroid hormone and supportive care begin within 2 hours of symptoms, survival rates jump to over 80%. Delays beyond 6 hours cut survival chances in half. Early recognition and immediate action are the biggest factors in recovery.
Why do doctors sometimes miss myxedema coma?
Because the symptoms mimic other conditions - especially in older adults. Confusion looks like dementia. Cold and fatigue look like aging. Slow breathing looks like sedation. Even low sodium can be blamed on diuretics or heart failure. Plus, many patients don’t have the classic swelling or hair loss. Without a high index of suspicion, it’s easy to overlook.
Should I check thyroid levels if I’m feeling unusually tired and cold?
If you have a history of thyroid disease or are on thyroid medication, yes - especially if you’ve had recent illness, surgery, or cold exposure. But if you’re feeling profoundly sluggish, cold, confused, or your heart rate is under 60 bpm without a known cause, treat it as an emergency. Don’t wait for a doctor’s appointment. Go to the ER.
Can myxedema coma happen to younger people?
Yes, though it’s rare. About 25% of cases occur in people under 60. Men are more likely to be misdiagnosed because doctors don’t expect hypothyroidism in them. Younger patients who stop their medication - especially during hospital stays - are at high risk. Even a few days without levothyroxine can trigger crisis in someone with long-standing disease.
What’s the difference between T4 and T3 in treatment?
Levothyroxine (T4) is the standard - it’s stable and converts to T3 in the body. But in severe cases, especially with heart or lung failure, the body can’t convert T4 fast enough. That’s why adding liothyronine (T3) directly - which works immediately - improves outcomes. The 2022 Endocrine Society guidelines now recommend T3 in severe cases to speed up recovery and reduce death risk.






