For years, parents were told to wait until their child was two or three before giving them peanut butter. That advice came from well-meaning doctors who thought delaying exposure would prevent allergies. But something strange happened: the more people waited, the more kids developed peanut allergies. By 2010, nearly 1 in 50 children in the U.S. had a peanut allergy - up from just 1 in 250 in 1997. Then came a game-changing study. The LEAP study, published in 2015, flipped everything on its head. It showed that introducing peanut to babies as early as 4 months could cut their risk of developing a peanut allergy by up to 86%. Today, the science is clear: early exposure isn’t risky - it’s protective.
Why Early Introduction Works
Our immune system learns what’s safe by tasting things early and often. When peanut is kept away, the body doesn’t learn to recognize it as harmless. Instead, it sees peanut proteins as invaders and mounts a dangerous response - leading to hives, vomiting, breathing trouble, or even anaphylaxis. But when a baby eats peanut protein regularly starting at 4 to 6 months, their immune system builds tolerance. It’s like training a muscle. The more it sees peanut, the less it fears it.
The LEAP study followed 640 high-risk babies - those with severe eczema or egg allergy - from 4 to 11 months. Half were fed peanut-containing foods three times a week. The other half avoided peanut completely. By age 5, only 2% of the group that ate peanut developed an allergy. In the avoidance group? 14% did. That’s a 75% drop. Follow-up studies showed this protection lasted even after kids stopped eating peanut for a full year. This wasn’t just temporary desensitization - it was true tolerance.
Who Needs Early Introduction - and When
Not every baby needs the same approach. The current guidelines, set by the NIAID in 2017 and updated in 2023, divide infants into three risk groups:
- High-risk: Babies with severe eczema, egg allergy, or both. These infants should be evaluated by a doctor or allergist between 4 and 6 months. If testing shows no peanut allergy, they start eating 2 grams of peanut protein - about 2 teaspoons of smooth peanut butter - three times a week. The first dose is often given in the doctor’s office for safety.
- Moderate-risk: Babies with mild to moderate eczema. These kids can start peanut at home around 6 months, with no testing needed. Just mix smooth peanut butter into pureed fruit or cereal.
- Low-risk: Babies with no eczema or food allergies. Peanut can be introduced anytime after solids begin - usually around 6 months - just like any other new food.
The magic window is before 6 months. A 2023 meta-analysis of LEAP and EAT studies found that babies who started peanut before 6 months had a 98% lower chance of developing an allergy in the per-protocol group. Even those with mild eczema saw a 100% reduction. Delaying past 6 months cuts the benefit in half.
How to Safely Introduce Peanut
Never give whole peanuts or chunky peanut butter to babies. They’re choking hazards. Instead, use smooth peanut butter thinned with water, breast milk, or formula. Mix 2 teaspoons of peanut butter with 2-3 tablespoons of warm liquid until it’s runny. Stir it into oatmeal, apple sauce, or mashed banana. You can also use peanut puff snacks like Bamba - a popular choice in the LEAP study - which dissolve easily in the mouth.
Start small. Give a tiny amount - about 1/4 teaspoon - on the tip of a spoon. Wait 10 minutes. Watch for any reaction: rash, vomiting, swelling, or trouble breathing. If nothing happens, give the rest. Do this three times a week. Consistency matters more than quantity. Even if your baby spits it out or eats only half, keep trying. The goal is regular exposure, not perfection.
For high-risk babies, the first peanut feeding should happen under medical supervision. That doesn’t mean a hospital stay - most allergists will have you come in for a 30-minute observation. If your baby has a reaction, they’ll treat it immediately. But most don’t. In the LEAP study, over 90% of high-risk infants had no reaction during their first peanut exposure.

What About Oral Immunotherapy (OIT)?
Oral immunotherapy is not prevention - it’s treatment. If your child already has a peanut allergy, OIT may help them tolerate small amounts. It involves eating tiny, increasing doses of peanut protein daily under strict medical care. Over months or years, some kids can eat a few peanuts without a reaction. But OIT doesn’t cure the allergy. It just raises the threshold. If they stop taking the dose, the allergy often returns.
Unlike early introduction, which is safe and effective for healthy babies, OIT is risky. It carries a high chance of allergic reactions - even anaphylaxis. It’s only for children with diagnosed peanut allergy, and only under a specialist’s watch. It’s expensive, time-consuming, and not for everyone. Prevention through early exposure is simpler, safer, and far more effective.
Why So Many Parents Still Wait
Despite strong evidence, only about 39% of high-risk infants in the U.S. get early peanut exposure. Why? Fear. Confusion. Misinformation.
Many parents still believe peanut is dangerous for babies. Others don’t know their child is high-risk. Pediatricians themselves aren’t always up to date - a 2023 survey found only 54% of pediatricians knew the current guidelines. Some still tell parents to wait. Others give vague advice like “wait until you’re sure.”
There’s also a cultural gap. Black and Hispanic infants are 22% less likely to get early peanut exposure than white infants. This isn’t because of parenting choices - it’s because of unequal access to care, language barriers, and lack of targeted education.
And then there’s the peanut butter problem. Parents try to give straight peanut butter - too thick, too sticky. Or they use crunchy. Or they think “a little bit” means a lick. None of that works. You need smooth, diluted, consistent exposure. And you need to start early.
What’s Changed Since 2017
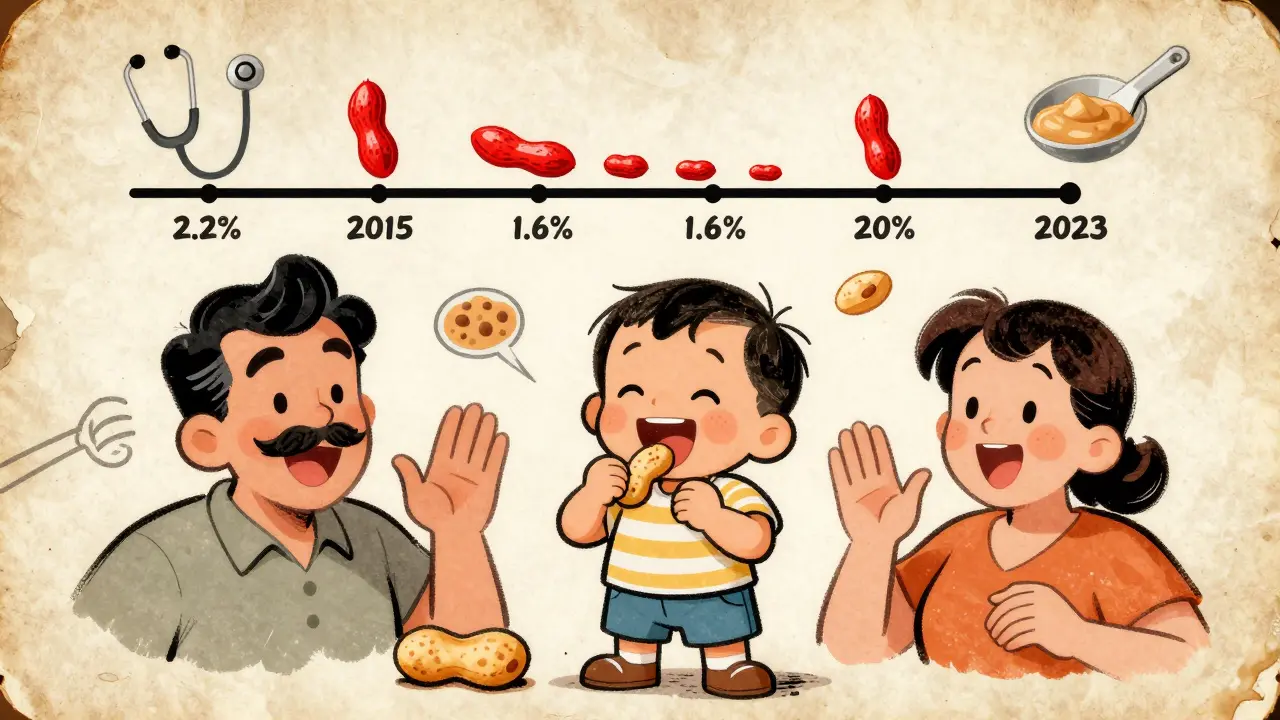
Since the guidelines came out, peanut allergy rates have started to drop. In 2015, 2.2% of U.S. children had peanut allergy. By 2023, that number fell to 1.6%. That’s about 300,000 fewer kids with a life-threatening condition. The biggest drop? In high-risk kids with eczema. Mild eczema: 85% fewer allergies. Moderate: 87% fewer. Severe: 67% fewer.
Researchers are now looking at whether introducing multiple allergens at once - peanut, egg, milk - gives even broader protection. Early results from the EAT study extension are promising. And the PRESTO trial, funded by the NIAID, is testing whether even lower doses of peanut protein, given even earlier, can prevent allergies in the highest-risk babies.
Meanwhile, the market is catching up. Peanut puff snacks, spoonable peanut butter pouches, and medical-grade infant peanut products have grown 27% a year since 2018. These aren’t gimmicks - they’re tools that make safe introduction easier for parents.
What You Can Do Today
If you’re a parent:
- Check your baby’s skin. Do they have eczema? Is it mild, moderate, or severe?
- Do they have an egg allergy? If yes, they’re high-risk.
- If high-risk, talk to your pediatrician before 4 months. Ask about referral to an allergist.
- If moderate or low-risk, start peanut at 6 months - no test needed.
- Use smooth peanut butter, thinned with water or milk. Mix it into food.
- Give it three times a week. Don’t stop if they spit it out.
- Watch for reactions. If you see swelling, vomiting, or trouble breathing, call 999 or go to A&E.
If you’re a doctor:
- Know the guidelines. Don’t wait for parents to ask.
- Ask about eczema and egg allergy at every 4- to 6-month checkup.
- Don’t say “wait and see.” Say “introduce now.”
- Offer a sample of diluted peanut butter. Show them how.
Frequently Asked Questions
Can I give my baby peanut butter straight from the jar?
No. Thick, chunky, or undiluted peanut butter is a choking hazard for babies under 1. Always mix smooth peanut butter with water, breast milk, or formula until it’s runny. You can also use peanut puff snacks like Bamba, which dissolve easily.
What if my baby has a reaction the first time?
Stop giving peanut immediately. If it’s mild - like a few hives or a rash - call your pediatrician. If it’s severe - swelling of the lips or tongue, vomiting, trouble breathing, or loss of consciousness - call 999 or go to the nearest emergency department. Most babies don’t react, but if they do, it’s not a reason to avoid peanut forever. Many can be safely reintroduced under medical supervision.
Is it too late if my child is already 1 year old?
The strongest protection happens before 6 months, but introducing peanut between 6 and 12 months still lowers risk. After 12 months, the benefit drops significantly. If your child is older and hasn’t had peanut, talk to your doctor. They may recommend testing first, especially if your child has eczema or other food allergies.
Do I need to keep feeding peanut forever?
Yes. Once your child is eating peanut regularly, keep giving it at least once a week. Stopping increases the chance the allergy will return. Studies show that consistent exposure is what keeps the immune system trained. Even after tolerance is built, regular intake matters.
Can I prevent peanut allergy by avoiding it during pregnancy?
No. Eating or avoiding peanut during pregnancy or breastfeeding doesn’t affect your baby’s risk. The only proven method is introducing peanut to the baby directly, starting at 4-6 months. Maternal diet has no significant impact according to Cochrane reviews.






Write a comment
Your email address will be restricted to us