When two drugs are supposed to do the same thing, how do you prove they work the same way in real patients? Traditional bioequivalence studies used to rely on healthy volunteers, with blood drawn every 15 to 30 minutes over 24 hours. But that approach doesn’t reflect how drugs behave in actual patients - especially children, the elderly, or people with kidney or liver disease. Enter population pharmacokinetics (PopPK): a smarter, more realistic way to prove drug equivalence using sparse, real-world data from hundreds of patients.
Why Traditional Bioequivalence Falls Short
For decades, regulators accepted bioequivalence based on two numbers: AUC and Cmax. If the 90% confidence interval for the ratio of these values between two drug formulations fell between 80% and 125%, they were considered equivalent. Simple. Clean. But it had a big flaw - it assumed everyone responds the same way. That assumption breaks down fast in real life. A 70-year-old with reduced kidney function doesn’t clear a drug the same way a 25-year-old athlete does. A child weighing 15 kg needs a different dose than a 90 kg adult. Traditional studies often excluded these groups entirely. Even when they were included, small sample sizes meant you couldn’t tell if differences were due to the drug or just natural variation. PopPK changes the game. Instead of asking 24 healthy people to stay in a clinic for days, it uses data from hundreds of patients already receiving the drug in normal clinical care. Maybe they had one or two blood draws during routine monitoring. Maybe their doses varied. Maybe sampling times were irregular. PopPK doesn’t need perfect data - it’s built to handle messy, real-world conditions.How PopPK Works: The Math Behind the Magic
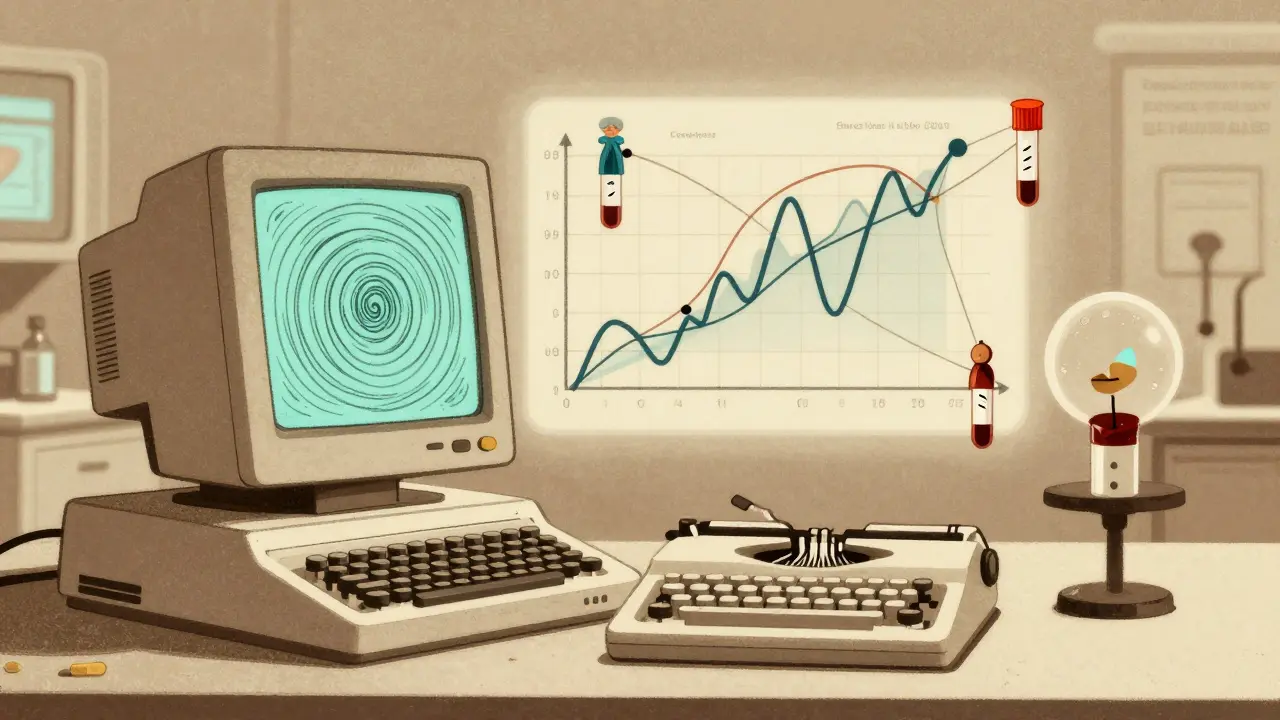
At its core, PopPK uses nonlinear mixed-effects modeling. Think of it as two layers of analysis. The first layer looks at each patient’s individual drug levels over time. The second layer looks at how those individual patterns fit into the bigger picture - the population. It doesn’t just calculate an average. It finds patterns. Why does Drug X clear faster in some people? Is it because of their weight? Their age? Their kidney function? PopPK identifies these factors - called covariates - and quantifies how much they affect drug exposure. If two formulations show nearly identical responses across all these variables, you can say they’re equivalent, even if the average AUC is slightly different. The key metrics PopPK tracks are between-subject variability (BSV) and residual unexplained variability (RUV). BSV tells you how much drug exposure differs naturally between people. For many drugs, BSV ranges from 10% to 60%. If the BSV between two formulations is within the same range, and the model shows no meaningful difference in how covariates affect them, you’ve got equivalence. The FDA’s 2022 guidance made this official: PopPK data can replace traditional bioequivalence studies in certain cases. They specifically mention situations where the patient population is highly variable and the therapeutic window is narrow - like with anticoagulants, anti-seizure drugs, or chemotherapy agents.Regulatory Shifts: From Skepticism to Standard Practice
PopPK isn’t new. The first real-world application was in 1977. But for years, regulators were cautious. They wanted clean, controlled data. It wasn’t until 2022 that the FDA published its first formal guidance on PopPK for equivalence claims. That document was a turning point. It didn’t just say “you can use PopPK.” It laid out exactly how to do it right: minimum sample sizes (40+ participants), required covariates, model validation steps, and reporting standards. Suddenly, companies had a roadmap. By 2021, about 70% of new drug applications included PopPK analyses - up from less than 20% a decade earlier. The EMA and Japan’s PMDA followed suit. Now, it’s not just about proving equivalence - it’s about proving it across subgroups. For example, a biosimilar for a cancer drug might be tested in 50 patients with varying levels of liver function. PopPK can show that exposure stays within safe limits across all of them. A traditional crossover study couldn’t do that without recruiting dozens of patients with rare conditions - which would be unethical or impossible.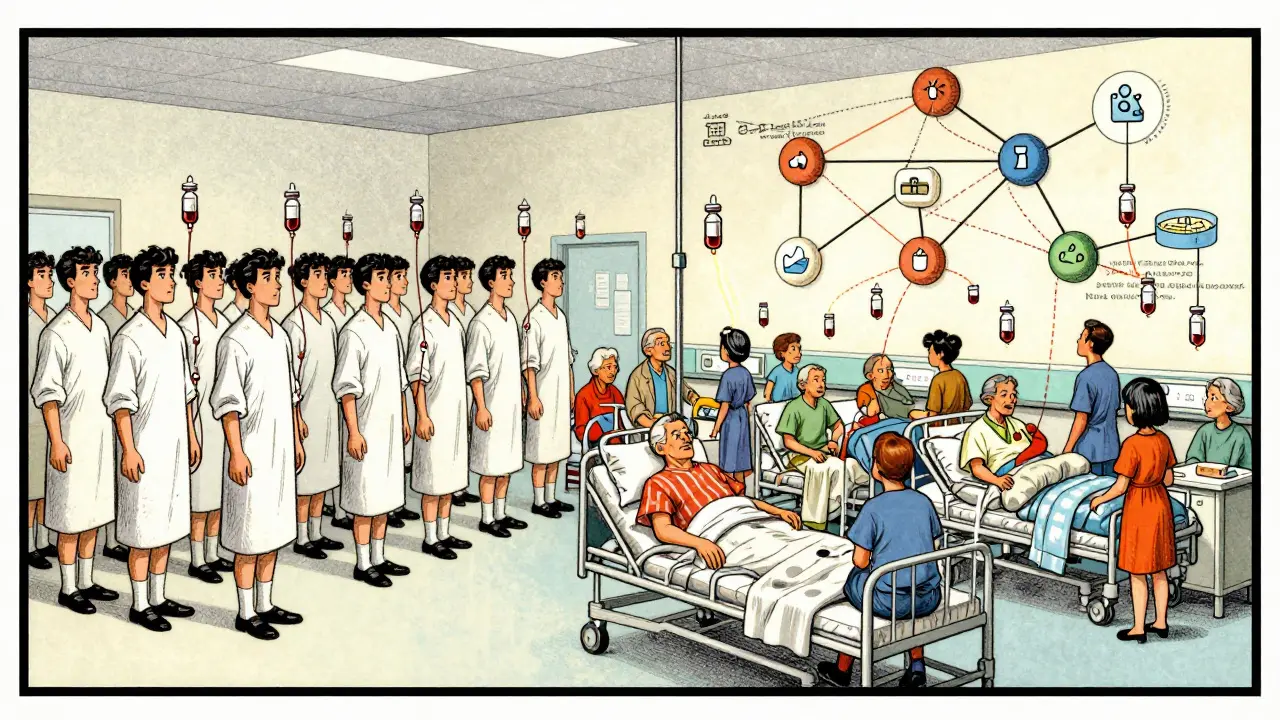
Tools of the Trade: Software and Skills
You can’t run PopPK in Excel. You need specialized software. NONMEM has been the industry standard since the 1980s and is still used in 85% of FDA submissions. Monolix and Phoenix NLME are also common. These tools handle the complex math behind mixed-effects modeling. But software alone isn’t enough. Building a valid PopPK model takes expertise. Pharmacometricians - specialists trained in both pharmacology and statistics - spend 18 to 24 months learning how to design models, avoid overfitting, and validate results properly. Many submissions get rejected not because the science is wrong, but because the model-building process wasn’t documented clearly enough. A 2019-2021 analysis of FDA Complete Response Letters found that 30% of PopPK submissions needed more information - mostly because of poor model justification or insufficient validation. The lesson? Transparency matters. You need to show every step: which covariates you tested, why you kept or dropped them, how you checked for bias, and how you confirmed the model works on data it hasn’t seen before.Where PopPK Shines: Real-World Examples
One of the biggest wins for PopPK has been in pediatric drug development. Getting blood samples from infants is hard. Ethical review boards won’t approve intensive sampling in newborns. But PopPK lets researchers use sparse data from children already on the drug - maybe from routine hospital monitoring - to build models that predict safe doses for babies who’ve never been studied before. Another example: drugs for patients with renal impairment. Traditional bioequivalence studies require giving the drug to people with severe kidney disease - risky if the drug has a narrow therapeutic window. PopPK can use data from patients with mild to moderate impairment and extrapolate to severe cases, using kidney function as a covariate. Pfizer and Merck have used this approach to support regulatory submissions without conducting additional clinical trials. Even in generics, PopPK is cutting costs. One company reported a 35% reduction in clinical trial costs by using PopPK to prove equivalence across weight and age groups instead of running separate studies for each subgroup.
Limitations and Challenges
PopPK isn’t a magic bullet. It struggles when data is too sparse - say, only one blood sample per patient with no covariate information. It also doesn’t replace traditional studies for drugs with extremely high variability, where replicate crossover designs still give more precise estimates of within-subject variation. There’s also a gap in standardization. While the FDA has clear guidelines, other agencies are still catching up. A 2023 Reddit post from a senior pharmacometrician noted that EMA committees sometimes demand more data than FDA reviewers - even for the same submission. That inconsistency creates headaches for global drug developers. And then there’s the human factor. Many clinical trials are designed without PopPK in mind. If sampling times aren’t planned, covariates aren’t recorded, or data is incomplete, you can’t go back and fix it. That’s why experts insist: PopPK planning must start in Phase 1, not Phase 3.The Future: Machine Learning and Global Harmonization
The next leap is coming from machine learning. A January 2025 study in Nature showed how AI models could detect hidden, non-linear relationships between patient traits and drug levels - things traditional PopPK models might miss. For example, a combination of low albumin and high inflammation might uniquely affect clearance, even if neither factor alone does. The IQ Consortium is working on standardizing validation protocols by late 2025. That’s a big deal. Right now, every company validates models differently. Once there’s a shared standard, regulators will trust PopPK even more. The global pharmacometrics market, fueled by PopPK, is expected to grow from $498 million in 2022 to over $1.2 billion by 2029. Nearly all top pharmaceutical companies now have dedicated pharmacometrics teams - up from just 65% in 2015. PopPK isn’t a niche tool anymore. It’s becoming the default way to understand how drugs behave in real people.Final Take: When to Use PopPK
Use PopPK when:- You’re developing drugs for heterogeneous populations (children, elderly, organ-impaired)
- The therapeutic window is narrow (e.g., warfarin, digoxin, tacrolimus)
- You’re developing biosimilars for large molecules where traditional studies are impractical
- You want to reduce trial costs and avoid unethical dosing in vulnerable groups
- The drug has very high within-subject variability
- You only have one or two data points per patient with no covariates
- You’re trying to prove equivalence for a drug with a wide therapeutic window and simple PK
What is the main advantage of population pharmacokinetics over traditional bioequivalence studies?
PopPK uses real-world, sparse data from hundreds of patients - including those with varying health conditions - to assess how a drug behaves across different subgroups. Traditional studies rely on small groups of healthy volunteers with intensive sampling, which doesn’t reflect how drugs work in real patients, especially children, the elderly, or those with organ impairment.
Can PopPK replace traditional bioequivalence studies entirely?
Yes, in specific cases - especially when the target population is highly variable and the drug has a narrow therapeutic window. The FDA and EMA now accept PopPK data as sufficient for equivalence claims in these scenarios. But for drugs with very high within-subject variability, traditional crossover designs still provide more precise estimates.
What software is used for population pharmacokinetic modeling?
NONMEM is the industry standard, used in 85% of FDA-submitted PopPK analyses. Other tools include Monolix and Phoenix NLME. These programs handle complex nonlinear mixed-effects modeling that can’t be done with standard statistical software.
Why is model validation so important in PopPK?
Because PopPK models are built on real-world data that’s often incomplete or noisy, validation ensures the model isn’t just fitting random noise. Without proper validation - like internal and external testing, residual analysis, and covariate stability checks - regulators will reject the submission. About 30% of PopPK applications require additional data due to poor validation.
How many patients are needed for a reliable PopPK analysis?
The FDA recommends at least 40 participants to ensure robust parameter estimation. But the real number depends on how much variability you expect and how strong the covariate effects are. More patients and more informative sampling (e.g., multiple time points per person) improve accuracy.
Is PopPK used only for small-molecule drugs?
No. PopPK is increasingly used for biologics and biosimilars, where traditional bioequivalence studies are impractical due to the size and complexity of the molecules. In fact, the biologics sector is one of the fastest-growing areas for PopPK applications.
What are the biggest challenges in implementing PopPK?
The top challenges are model validation (cited by 65% of pharmacometricians), lack of standardized protocols, and poor data quality from trials not designed with PopPK in mind. Getting enough covariate data - like weight, age, kidney function - is often harder than running the model itself.
How early should PopPK be planned in drug development?
Ideally, in Phase 1. That’s when you design the clinical trial to collect the right kind of data - sparse samples, recorded covariates, and consistent timing. Waiting until Phase 3 makes it nearly impossible to go back and fix missing information.

Write a comment
Your email address will be restricted to us