When a drug goes straight into your bloodstream, there’s no second chance. No stomach acid to kill contaminants. No immune system on standby. That’s why sterile manufacturing for injectables isn’t just about cleanliness-it’s about survival. A single bacterium in a vial can trigger sepsis, organ failure, or death. The 2012 meningitis outbreak linked to contaminated steroid injections killed 64 people and sickened over 750. That tragedy didn’t come from negligence alone-it came from gaps in understanding what true sterility really means.
Why Sterility Isn’t Optional
Oral pills dissolve in the gut. The body handles most contaminants naturally. Injectables don’t get that luxury. They enter the blood, the cerebrospinal fluid, or tissues directly. That’s why regulatory agencies demand a sterility assurance level (SAL) of 10^-6. That means, statistically, no more than one contaminated product in a million. It’s not a target-it’s the floor. The World Health Organization set this standard in 2011, and since then, every major regulator-from the FDA to the EMA-has locked it in.The consequences of failure are brutal. In 2022, the FDA cited 1,872 violations in sterile manufacturing facilities-up from 1,245 in 2019. Over two-thirds of those were tied to aseptic technique failures. Not equipment. Not design. Human error during filling. Glove tears. Improper gowning. Uncontrolled airflow. These aren’t theoretical risks. They’re daily realities in facilities that cut corners.
Two Paths to Sterility: Terminal vs. Aseptic
There are only two ways to make injectables sterile: terminal sterilization or aseptic processing. And they’re not interchangeable.Terminal sterilization means you make the product, seal it, then blast it with heat or radiation. Steam at 121°C for 15-20 minutes kills everything. Gamma radiation at 25-50 kGy does the same. This method is reliable, validated, and cheaper-around $50,000 per batch. But here’s the catch: only 30-40% of injectables can survive it. Biologics like monoclonal antibodies, mRNA vaccines, and protein-based therapies? They fall apart under heat or radiation. That’s why 70% of new injectable drugs today can’t use terminal sterilization.
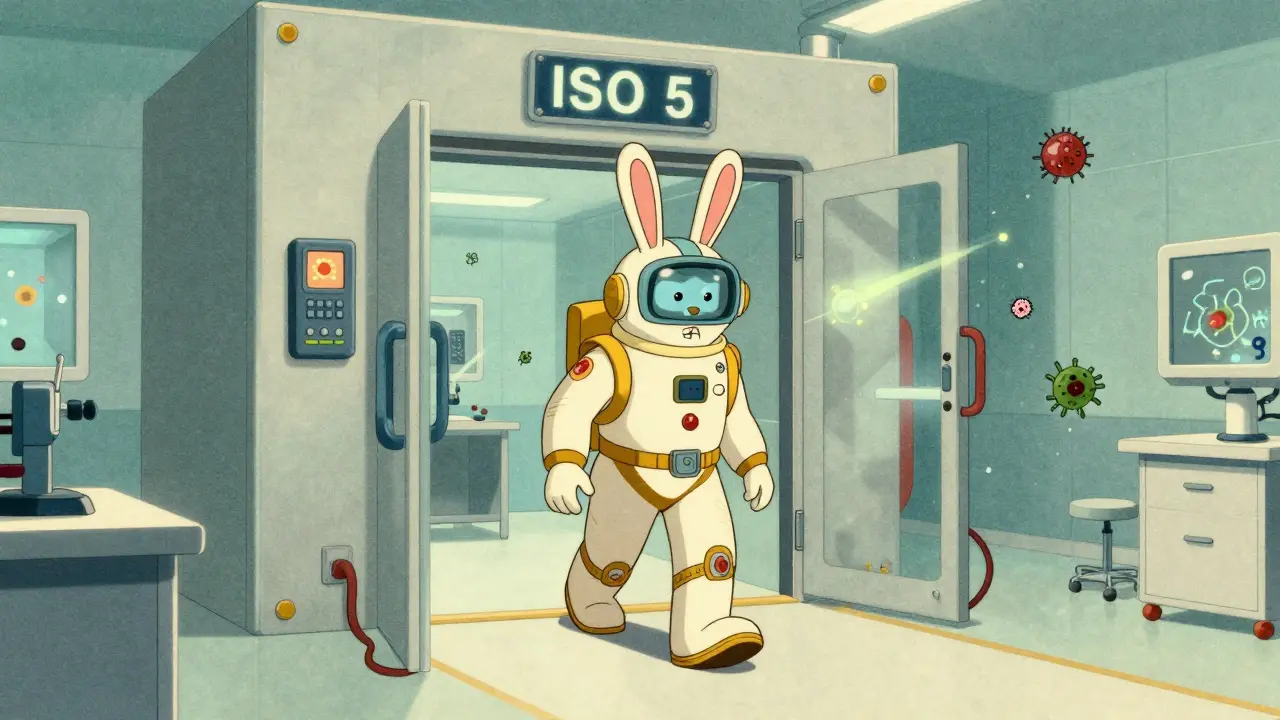
That leaves aseptic processing. No heat. No radiation. Everything stays sterile from raw material to final seal. This is where things get intense. You need an ISO 5 cleanroom-the cleanest environment humans can build. That’s 3,520 particles per cubic meter, no larger than 0.5 microns. For context: a typical office has over 10 million particles per cubic meter. In an ISO 5 zone, you’re breathing air cleaner than the surface of Mars.
To maintain that, you need RABS (Restricted Access Barrier Systems) or isolators. RABS are enclosed workstations with gloves built into the walls. Isolators are fully sealed chambers with robotic arms. Both keep people out of the critical zone. Isolators reduce contamination risk by 100 to 1,000 times compared to open cleanrooms, but they cost 40% more to install. RABS are cheaper and easier to operate-but if the gloves tear or the airflow stalls, you’re exposed.
Environment Is Everything
It’s not enough to have a cleanroom. You have to prove it’s working-every minute.ISO 14644 standards require continuous monitoring. Particle counters run nonstop. Air samplers trap microbes. You don’t wait for a test result-you react in real time. In ISO 5 areas, the alert level for airborne bacteria is 1 colony-forming unit (CFU) per cubic meter. The action level? 5 CFU/m³. Go over that, and you stop production. No exceptions. That’s why facilities now install sensors on every wall, every filling line, every glove port.
Pressure differentials matter too. Rooms must be kept at 10-15 Pascals higher pressure than the next room. Air flows inward, never outward. Temperature and humidity? Held steady at 20-24°C and 45-55% RH. Too dry? Static builds up. Too humid? Condensation forms. Both can carry particles into the product.
Water isn’t just purified-it’s Water for Injection (WFI). It must have less than 0.25 endotoxin units per milliliter. Containers? They’re depyrogenated at 250°C for 30 minutes. That’s not cleaning. That’s incinerating the DNA of any leftover pyrogens.
The Human Factor
No matter how good the tech is, people still cause 70% of failures.Personnel training isn’t a one-time event. It’s 40-80 hours of hands-on practice, followed by media fill qualifications every six months. A media fill is a mock run: you fill containers with growth media instead of drug, incubate them, and see if anything grows. If even one vial turns cloudy, your entire process is suspect. The FDA says media fill failure rates above 0.1% mean your aseptic technique is broken.
One manager at a top pharma company lost $450,000 in a single batch because a glove in their RABS system had a microscopic tear. No one saw it. The machine didn’t flag it. The media fill passed. But the product? Contaminated. That’s why visual inspection now often uses automated systems. One company cut defects from 0.2% to 0.05% by switching to AI-powered cameras that spot tiny particles or misaligned stoppers. It cost $2.5 million-but saved millions in recalls.
Costs, Compliance, and the New Reality
Building a sterile injectable facility isn’t a project. It’s a $50-100 million commitment. You’re not just buying equipment-you’re buying validation, documentation, training, and monitoring systems that never sleep.EU GMP Annex 1, updated in 2022, changed the game. It forced companies to move from periodic environmental checks to continuous monitoring. It required Quality Risk Management (ICH Q9). It demanded real-time data, not batch summaries. Facilities that ignored this are now getting shut down.
CDMOs (contract manufacturing organizations) now handle 55% of sterile injectable production. Why? Because few companies can afford the capital or the expertise. Catalent, Lonza, and Thermo Fisher control 42% of that market. For startups, outsourcing isn’t optional-it’s survival.
But even big players struggle. In 2023, 68% of sterile manufacturing facilities reported at least one sterility test failure. The average cost? $1.2 million per incident. That’s not just lost product-it’s lost time, lost trust, lost regulatory standing.
What’s Next?
The future is automation, digital twins, and rapid testing. Closed processing systems-where materials move through sealed tubes without human contact-are now in 65% of new facilities. Robotic filling lines are growing at 40% per year. Rapid microbiological methods are cutting test times from 14 days to 24 hours. AI is being used to predict contamination risks before they happen.But the core hasn’t changed. Sterile manufacturing for injectables is still about one thing: protecting patients from invisible threats. The tools have evolved. The stakes haven’t.
If you’re producing injectables, you’re not just making a drug. You’re making a promise. And every vial, every line, every glove, every sensor-every single step-must be built to honor that promise.




Write a comment
Your email address will be restricted to us