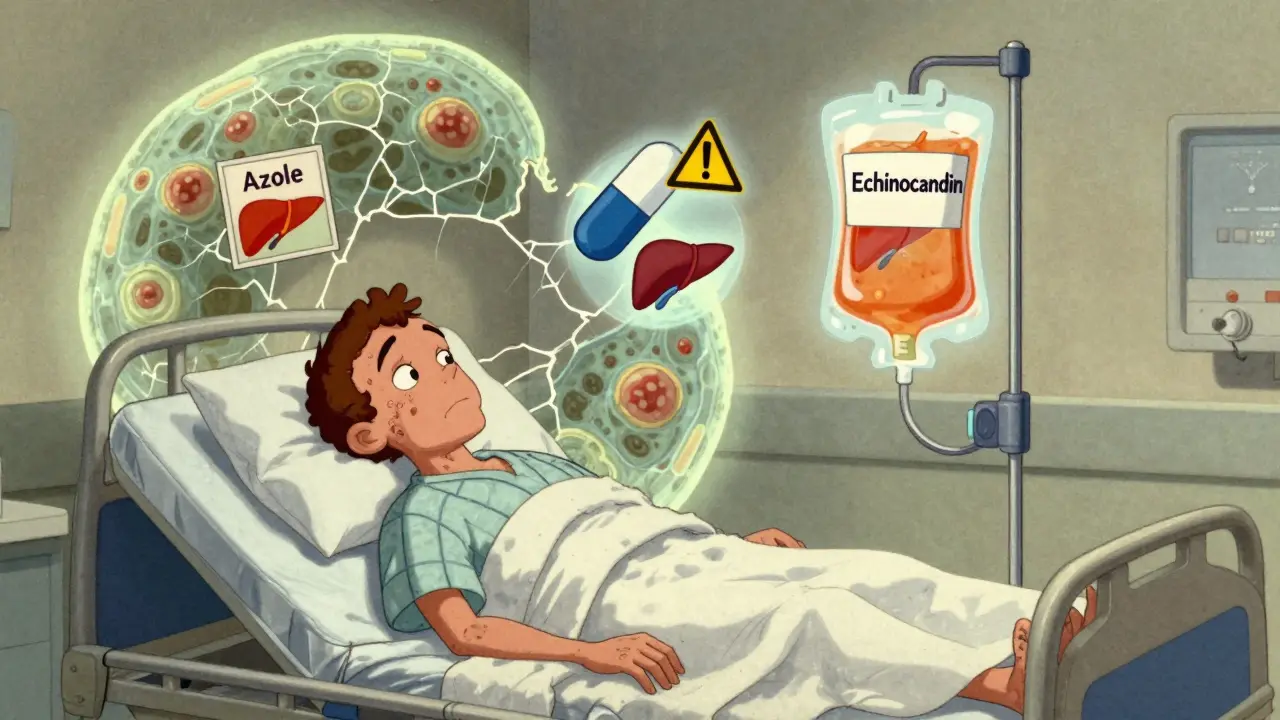
When a fungal infection turns serious, it’s not just about itching or a rash anymore. It’s about survival. Fungal infections like invasive candidiasis or aspergillosis can kill faster than many people realize-especially in hospitals, ICUs, or among those with weakened immune systems. That’s where antifungal medications come in. But not all are the same. Two major classes-azoles and echinocandins-dominate modern treatment, each with distinct strengths, risks, and real-world trade-offs.
How Azoles Work and When They’re Used
Azoles are the workhorses of antifungal therapy. Drugs like fluconazole, voriconazole, itraconazole, and posaconazole block a key enzyme in fungi called lanosterol 14-alpha-demethylase. Without this enzyme, fungi can’t build strong cell membranes. Their walls fall apart, and the infection dies. It’s simple, effective, and-most importantly-many of these drugs work orally.
Fluconazole is the most common. It’s cheap, well-absorbed (90% of an oral dose gets into your bloodstream), and works great for yeast infections like candidemia. In fact, studies show it cures about 82% of cases. But it’s not perfect. About 12% of people on fluconazole develop liver damage, compared to just under 5% on echinocandins. That’s a big difference when you’re treating someone already sick.
Voriconazole is the go-to for aspergillosis, a deadly lung infection common in transplant patients. It’s more powerful than older drugs like amphotericin B, cutting death rates from over 50% down to about 30%. But it comes with a strange side effect: 38% of people see blurry vision, light sensitivity, or color distortion. It’s temporary, but terrifying if you don’t know it’s coming. And it’s not just visual-voriconazole interacts with over 100 other drugs, including common ones like phenytoin and warfarin. One doctor in Manchester reported three cases where voriconazole doubled phenytoin levels in just two days, nearly causing seizures.
Echinocandins: The IV-Only Powerhouse
If azoles are the oral Swiss Army knife, echinocandins are the ICU specialist. Caspofungin, micafungin, and anidulafungin don’t attack cell membranes. They smash the fungal cell wall by blocking glucan synthesis-something human cells don’t even have. That’s why they’re so safe for people. No human cells, no damage.
But here’s the catch: you can’t swallow them. They’re given only through an IV. That means hospital stays, IV lines, and nursing time. They cost more too-caspofungin runs about $1,250 for a week’s course. Fluconazole? $150.
But for critically ill patients, that cost is worth it. In septic shock, echinocandins reduce kidney injury risk by over 85% compared to azoles. That’s not just a statistic-it’s the difference between needing dialysis or walking out of the hospital. The IDSA guidelines say: if someone is in the ICU with invasive candidiasis, start with an echinocandin. Not azole. Not amphotericin. Echinocandin.
And they’re cleaner in other ways. Only about 180 severe drug interactions are linked to echinocandins. Azoles? Nearly 600. That’s because azoles interfere with liver enzymes that break down everything from blood thinners to antidepressants. A patient on fluconazole and statins might end up with rhabdomyolysis. A patient on voriconazole and a heart rhythm drug could develop a dangerous QT prolongation. Echinocandins? Almost no such risks.
Drug Interactions: The Silent Killer
One of the most dangerous things about azoles isn’t the infection-it’s what else you’re taking. They’re notorious for messing with the CYP3A4 and CYP2C9 liver enzymes. That means common drugs like simvastatin, cyclosporine, tacrolimus, and even some antidepressants can build up to toxic levels.
A 2020 study of nearly 7,000 patients found that 86% to 93% of those on mold-active azoles had at least one drug interaction. Nearly a third were outright dangerous. One patient on posaconazole and clarithromycin developed a QT interval longer than 500ms-enough to trigger sudden cardiac arrest. The European Medicines Agency now requires baseline ECGs for high-risk patients.
Doctors in the UK are starting to check drug interaction databases before prescribing azoles. Some hospitals use automated alerts in their electronic systems. But many still miss it. A nurse in Manchester told me she once saw a patient on fluconazole and warfarin bleed internally because the INR shot up to 12. No one checked the interaction.

Monitoring and Safety Protocols
You can’t just hand someone an azole and send them home. Monitoring is non-negotiable.
The FDA requires quarterly liver tests for anyone on azoles. If ALT or AST levels rise above five times the normal limit, you stop the drug immediately. That’s not a suggestion-it’s a rule. In one hospital, 14% of patients on voriconazole needed dose changes because their liver enzymes climbed too high.
Therapeutic drug monitoring is also key. Voriconazole levels vary wildly between patients. One person might need 200mg twice daily; another might need 300mg just to hit the target range of 1-5.5 μg/mL. Without checking levels, you’re guessing. And guessing with antifungals can be deadly.
Echinocandins need less monitoring. Only patients with severe liver disease (Child-Pugh Class C) need dose adjustments. Micafungin gets halved in those cases. That’s it.
Special Populations: Pregnancy, Kids, and the Elderly
Pregnant women face a tough choice. Azoles are Category D-meaning there’s clear evidence of fetal harm. Birth defects have been reported. Echinocandins are Category C-risk can’t be ruled out, but no human data shows harm. In practice, echinocandins are preferred in pregnancy when systemic antifungals are needed.
For kids, fluconazole is often used for thrush or candidiasis. But voriconazole dosing is tricky-it changes with weight, age, and even liver maturity. Kids under 12 often need higher doses per kilogram than adults.
Older adults are at higher risk for kidney and liver issues. Azoles can pile up in their systems. Echinocandins are often safer, but IV access can be hard in frail patients. That’s why topical antifungals are still the first line for nail or skin infections-even in the elderly.

Resistance and the Future
Antifungals aren’t invincible. Resistance is rising. In Aspergillus fumigatus, azole resistance jumped from 1.8% in 2012 to 8.4% in 2022. Why? Agricultural use of triazole fungicides in crops. The same chemicals used to protect wheat and barley are breeding resistant fungi that infect humans.
And Candida auris-a drug-resistant yeast-is now a global threat. It spreads in hospitals, resists multiple antifungals, and kills up to 60% of infected patients. That’s why new drugs are urgent.
Rezafungin, a new echinocandin approved in March 2023, is a game-changer. It’s given once a week instead of daily. That cuts hospital stays and nursing burden. And olorofim, a brand-new class called an orotomide, just got breakthrough status from the FDA. In trials, it worked in 56% of patients who had failed all azoles.
Big pharma is investing too. AstraZeneca bought Fusion Pharmaceuticals for $3.2 billion last year, betting on next-gen antifungals. The market is expected to hit $21 billion by 2028.
What This Means for You
If you’re prescribed an azole, ask: What am I taking it for? What else am I on? Do I need liver tests? Don’t assume it’s safe just because it’s a pill. If you’re in the ICU and someone suggests an echinocandin, know it’s not about cost-it’s about survival.
Topical antifungals like clotrimazole are still safe for athlete’s foot or yeast infections. But if your infection is deep, systemic, or worsening, the choice between azole and echinocandin isn’t academic. It’s life or death.
Doctors aren’t choosing between drugs because they’re trendy. They’re choosing based on your liver, your kidneys, your other meds, your age, and whether you’re in a hospital bed or sitting at home. That’s why knowing the difference matters.
Are azoles safe for long-term use?
Azoles can be used long-term for chronic infections like aspergillosis or recurrent candidiasis, but only with strict monitoring. Liver function tests must be done every 3-6 months. Long-term use increases the risk of liver damage, drug interactions, and resistance. Fluconazole is the most tolerable for extended use, but voriconazole and posaconazole carry higher risks. Always discuss duration and alternatives with your doctor.
Why are echinocandins only given by IV?
Echinocandins are large molecules that don’t absorb well through the gut. If you swallow them, they pass through your system unchanged. That’s why they’re designed for IV delivery only. Researchers are working on oral versions, but none are approved yet. For now, if you need an echinocandin, you’ll need a port or IV line.
Can I take over-the-counter antifungals with prescription ones?
Be very careful. Topical antifungals like creams or sprays are generally safe because they don’t enter your bloodstream. But some OTC products combine antifungals with steroids-like clotrimazole-betamethasone. Using these while on systemic azoles can mask symptoms or worsen deep infections. Always tell your doctor about everything you’re using, even if it’s just a cream.
Do antifungals cause nausea?
Yes, especially azoles. Around 42% of people on fluconazole report nausea, and 29% have abdominal pain. Echinocandins cause less nausea (under 25%), but they can trigger infusion reactions-flushing, fever, or chills during the IV drip. Taking them slower or with antihistamines often helps. If nausea is severe, ask about anti-nausea meds or switching to a different antifungal.
What happens if I miss a dose of my antifungal?
For azoles like fluconazole, missing one dose isn’t usually dangerous-take it as soon as you remember, unless it’s close to the next dose. For voriconazole or posaconazole, timing matters more because levels need to stay steady. Missing doses can lead to treatment failure or resistance. Echinocandins are given daily or weekly; if you miss one, contact your provider immediately. Don’t double up. Always follow your prescriber’s instructions.




Write a comment
Your email address will be restricted to us