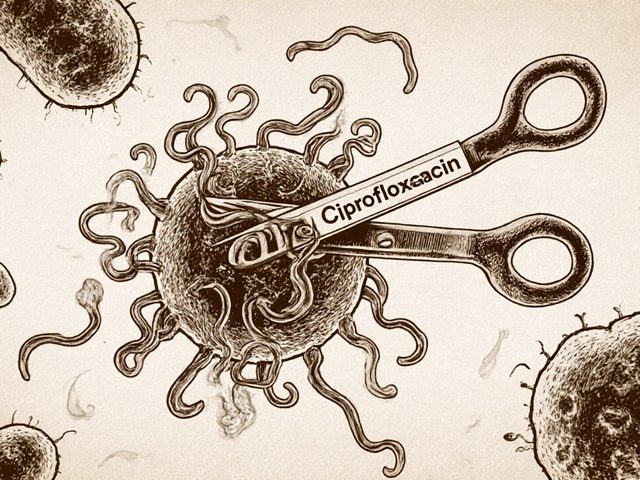
After surgery, you’re often given short-term medications to manage pain, prevent infection, or control other symptoms. These drugs-like painkillers, antibiotics, or muscle relaxants-are crucial for recovery. But they can also be dangerous if used incorrectly. Medication safety after surgery isn’t optional. It’s the difference between a smooth recovery and a life-threatening mistake.
Why Medication Errors Happen After Surgery
Most people assume hospitals are perfectly safe. But the truth is, surgical settings are high-pressure zones where mistakes happen more often than you think. According to the Joint Commission, 30% of all medication errors occur during surgery or in the immediate recovery period. Why? Because things move fast. Doctors give verbal orders. Nurses juggle multiple patients. Syringes get mixed up. Labels get missed. The World Health Organization reports that about 20% of all adverse events in surgery are tied to medication errors. And 35% of those lead to real harm-like allergic reactions, overdose, or organ damage. Even something as simple as a mislabeled syringe can cause a patient to get ten times the right dose of a powerful drug like fentanyl or morphine.The Core Rules: What You Must Do
There are non-negotiable steps that every medical team must follow. These aren’t suggestions. They’re science-backed, life-saving protocols.- One syringe, one patient, one use. The CDC says this clearly: never reuse a syringe-even for the same person. If you draw up pain medicine, use it right away. Discard the syringe after. Leaving it on the table or setting it down for “just a minute” is a major risk.
- Label everything. Any medication on the sterile field must be labeled with the drug name, strength, and expiration time. If it’s not labeled, it gets thrown out. No exceptions. Unlabeled vials or syringes are the leading cause of wrong-drug errors.
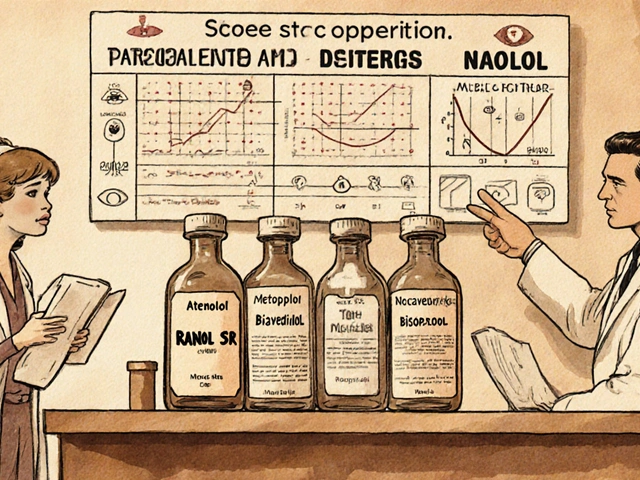
- Double-check high-alert drugs. Opioids, insulin, heparin, and neuromuscular blockers are called “high-alert” for a reason. One wrong dose can kill. Before giving any of these, two trained staff must verify the name, dose, and route. This isn’t just good practice-it’s required by the American Society of Anesthesiologists.
- Use read-backs. When a doctor says, “Give 5 mg of morphine IV,” the nurse must repeat it back: “Five milligrams of morphine, intravenous, correct?” This simple step cuts verbal order errors by 55%, according to ACOG.
What Gets Left Out (And Why It’s Dangerous)
Many facilities skip key steps because they’re “too slow” or “too much paperwork.” But skipping these steps isn’t efficiency-it’s gambling with lives. For example, some teams pre-label empty syringes before filling them. That’s a huge red flag. If you label a syringe as “0.5 mg epinephrine” before drawing it up, and you accidentally draw 5 mg instead? You’ve just created a time bomb. The ISMP 2022 guidelines ban this completely. Labels go on only after the drug is in the syringe. Another common mistake: storing medications in unlocked carts or on open trays. The ASA says all drugs must be kept in a secure, accessible area. Why? Because theft, tampering, or accidental mixing can happen in seconds. A 2023 ECRI report found that 19% of medication errors came from unlabeled or improperly stored drugs.
How to Spot a Risky Situation
You don’t need to be a nurse to notice danger. If you’re a patient or family member, watch for these warning signs:- A syringe or vial without a label.
- Someone preparing a drug while talking to another person-no eye contact, no confirmation.
- Multiple vials of the same drug with different colors or concentrations on the same tray.
- A nurse or tech rushing to give a drug right before the patient is moved.
What Happens When Rules Are Followed
The data doesn’t lie. Hospitals that fully implement these protocols see dramatic drops in errors. One study published in the AORN Journal found a 63% reduction in medication mistakes after staff started using verbal confirmation and strict labeling. Another facility cut errors by 47% just by making sure every syringe was labeled before leaving the sterile field. Even small changes add up. A 2022 AST survey showed that 78% of surgical technologists felt more confident in their work after training on medication safety. Why? Because they weren’t guessing anymore. They had clear steps.
What’s Changing in 2026
New tech is making this even safer. Barcode scanners are now being tested in operating rooms to match the drug with the patient’s wristband. Smart syringes are in development-they’ll refuse to deliver the wrong dose. And the CDC just updated its 2023 guidelines to require facemasks during spinal injections to prevent contamination. The ISMP is also rolling out specialty guides this year-orthopedic and cardiac versions-to tackle the unique risks in those areas. For example, in knee surgery, different concentrations of epinephrine are used for bleeding control. A mix-up here can cause heart rhythm problems. These new guides will make sure those risks are covered.What You Can Do as a Patient
You’re not powerless. Here’s how to protect yourself:- Ask: “What drug is this, and why am I getting it?”
- Watch the nurse or tech label the syringe. If they don’t, ask them to.
- If you’re getting multiple doses, ask: “Will you be using a new syringe each time?”
- At discharge, get a written list of all medications you’re taking, with dosages and times.
Final Reality Check
Medication safety after surgery isn’t about perfection. It’s about systems. One person forgetting a label won’t kill someone. But a culture that accepts it? That does. The numbers are clear: 1,247 medication errors were reported in just 2.5 years in surgical settings. 32% were wrong drugs. 28% were wrong doses. 19% were unlabeled. These aren’t rare accidents. They’re preventable failures. The good news? We know exactly how to fix them. It’s not about hiring more staff. It’s about sticking to the basics: label everything, verify everything, discard everything after one use. And never, ever assume someone else checked it.Can I reuse a syringe for multiple doses during the same surgery?
No. Even if it’s for the same patient, a syringe used for one dose must be discarded immediately after use. The CDC’s 2023 guidelines state that syringes must never be left unattended and must be thrown away after the procedure ends. Reusing a syringe-even briefly-increases the risk of contamination and dosing errors.
Why are some medications labeled differently on the surgical field?
Different concentrations are used for different procedures. For example, epinephrine for ear surgery might be 1:100,000, while for a major bleed, it could be 1:10,000. If both are on the same tray without clear labels, a mix-up can be deadly. The AST requires staff to verbally confirm strength before passing any medication with multiple concentrations.
What should I do if I notice a medication isn’t labeled?
Don’t assume it’s okay. Politely ask the nurse or tech to confirm the drug and dose. If they can’t, request that the medication be discarded and a new, properly labeled one be prepared. Most hospitals have policies that require this, and staff are trained to respond without defensiveness.
Are oral medications safer than injections after surgery?
Not necessarily. While injections carry higher risks during administration, oral meds can still be dangerous if the wrong drug or dose is given. For example, giving a patient a high-dose opioid pill instead of an antibiotic can lead to respiratory arrest. The same labeling and verification rules apply.
How do I know if my hospital follows safe medication practices?
Ask if they follow the ISMP 2022 Guidelines for Perioperative Medication Safety. Facilities that do will have labeled syringes, two-person verification for high-alert drugs, and no unlabeled medications on the field. You can also ask if they’ve had any medication error incidents in the past year-hospitals are required to track this.