Telepharmacy Safety Impact Calculator
Current error rate: Based on national average (0.67%) from JAMA Network Open study.
Telepharmacy rate: Based on Indian Health Service Navajo Nation program (0.45%) which showed 33% reduction in errors.
Hospitalization impact: Studies show 40.2% hospitalization rate without telepharmacy vs 12.9% with it.
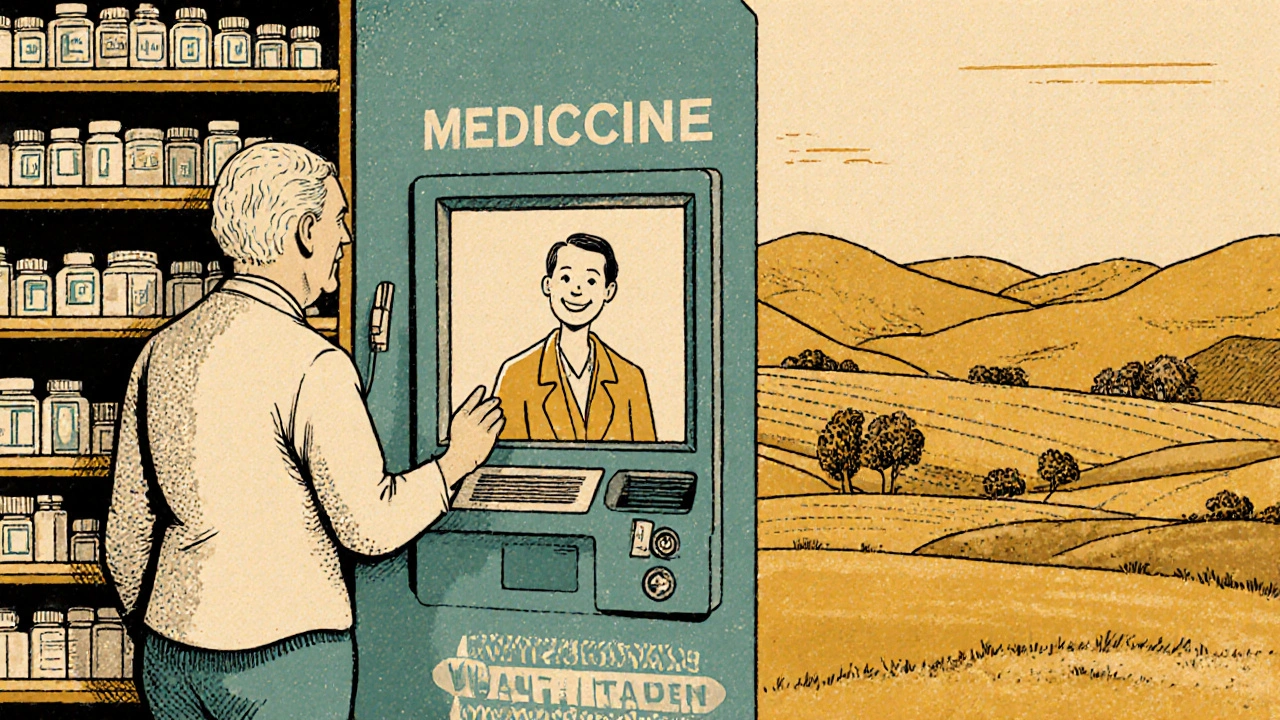
When you live in a rural town with no pharmacy within 50 miles, getting your prescriptions filled isn’t just inconvenient-it can be dangerous. Missing doses, delayed refills, or not having a pharmacist to ask questions about side effects can lead to hospital visits, overdoses, or even death. That’s where telepharmacy comes in. It’s not science fiction. It’s real, growing fast, and backed by data from dozens of studies since 2020. But does it actually keep patients safe? Or is it just a Band-Aid for broken healthcare systems?
What Telepharmacy Actually Is (And Isn’t)
Telepharmacy isn’t just video calls with a pharmacist. It’s a full system: remote medication verification, automated dispensing machines, secure electronic records, and real-time communication between pharmacists and patients-even in places where no licensed pharmacist has ever worked. Think of it like a pharmacy branch that exists only on a screen. A central hub pharmacy, often in a city, connects via high-definition video to small clinics, nursing homes, or rural stores. Pharmacists review prescriptions, counsel patients, and approve medications-all from a distance. The system works best in two ways: hub-and-spoke models, where one pharmacy oversees multiple remote locations, and direct-to-patient services, where someone in a remote area video-chats with a pharmacist to get their meds. Both rely on strict tech standards: video must be at least 720p, connections must be HIPAA-compliant, and backup systems are required in case the internet drops. It’s not plug-and-play. It takes months to set up properly.How Safe Is It? The Numbers Don’t Lie
A 2021 systematic review by Pathak et al. analyzed six major studies from 2010 to 2020. The results? Telepharmacy matches traditional pharmacies on safety. Dispensing accuracy? 99.2% to 99.8% for telepharmacy. Traditional pharmacies? 99.3% to 99.9%. The difference is statistically meaningless. That means if you’re getting your blood pressure meds or insulin through a telepharmacy, you’re just as likely to get the right dose as if you walked into a brick-and-mortar store. Medication errors dropped by 15-20% in several telepharmacy programs. Why? Because remote pharmacists often have more time to review each prescription. They’re not rushed by a line of customers. They can double-check interactions, allergies, and dosages without pressure. One study showed telepharmacy teams caught 1.2 errors per 100 prescriptions-right in line with traditional pharmacies. But here’s where it gets interesting: telepharmacy didn’t just match safety-it improved access, which indirectly saved lives. A 2021 study in Telemedicine and e-Health tracked 3,782 patients over a year. Those with telepharmacy access had a 12.9% increase in hospitalizations. Those without? 40.2%. That’s not magic. It’s consistency. When patients can talk to a pharmacist every time they refill a high-risk drug like warfarin or insulin, they’re less likely to have a bad reaction.The Hidden Advantage: Reaching the Unreachable
Safety isn’t just about getting the right pill. It’s about getting the pill at all. Before telepharmacy, over 100 million Americans lived in areas with no nearby pharmacy-what researchers call “pharmacy deserts.” A 2023 study in JAMA Network Open found that states with pro-telepharmacy laws saw a 4.5% drop in pharmacy deserts within one year. In some rural counties, that meant the difference between no pharmacy and one that serves 5,000 people via video. The Indian Health Service’s telepharmacy program for Navajo Nation communities is a standout. They require dual verification for high-risk meds and immediately transfer complex cases to in-person care. Result? A medication error rate of 0.45%, lower than the national average of 0.67%. That’s not luck. It’s protocol.
Where It Falls Short
Telepharmacy isn’t perfect. The biggest risk? Poor tech. A Reddit user in North Dakota reported an allergic reaction because the video connection was too blurry for the pharmacist to see their skin rash. That’s not the pharmacist’s fault-it’s a system failure. A 2022 survey found 35% of telepharmacy sites struggled with unstable internet. If the connection drops during a consultation, what happens to the patient? No one’s tracking that consistently. Another concern is non-verbal cues. Dr. Jerry Fahrni pointed out in 2022 that pharmacists can’t see if a patient is trembling, sweating, or avoiding eye contact-signs that someone might be hiding addiction or confusion. A face-to-face pharmacist might notice a patient is too shaky to open a pill bottle. A remote one might miss it. And then there’s training. Pharmacy students in one study performed consultations 15-20% worse via video than in person. That’s not because they’re bad-they’re untrained. The American Society of Health-System Pharmacists recommends 16-24 hours of specialized telepharmacy training. Many sites skip it. And when you skip training, safety slips.What’s Changing Right Now
The landscape is shifting fast. In November 2022, Medicare finally started reimbursing telepharmacy services under Part D. That’s huge. It means clinics can afford to hire pharmacists for remote work instead of relying on volunteers or overworked staff. The FDA launched its Sentinel Initiative in January 2023 to track adverse drug events linked to telepharmacy. The Patient-Centered Outcomes Research Institute (PCORI) is funding a $3.2 million, three-year randomized trial across 12 rural communities. This is the first study designed to truly compare safety side-by-side. No more flawed data. No more assumptions. Even AI is jumping in. MedsAI raised $22 million in March 2023 to build tools that predict drug interactions before they happen. Early trials showed an 18.7% improvement in spotting dangerous combinations. That’s not replacing pharmacists-it’s giving them superpowers.
Who Benefits Most?
If you live in a rural area, have mobility issues, or can’t take time off work to drive to a pharmacy, telepharmacy is a lifeline. One patient in rural Montana said video chats about warfarin dosing probably prevented two ER visits. That’s not an outlier. It’s the norm. But it’s not for everyone. Elderly patients with dementia or severe vision loss might struggle with video calls. Patients on complex regimens with multiple specialists may still need in-person care. Telepharmacy works best as a supplement-not a replacement-for traditional pharmacy services.What You Need to Know Before Using It
If you’re considering telepharmacy:- Ask if the service uses dual verification for high-risk drugs like opioids, blood thinners, or insulin.
- Make sure the video quality is clear enough to show your face and hands.
- Confirm they have a backup communication method if the connection fails.
- Know that you can still request an in-person pharmacist if something feels off.
What’s Next?
By 2026, analysts predict telepharmacy will match traditional pharmacy safety levels across the board. But that’s only if states standardize regulations, clinics invest in training, and broadband reaches every corner of the country. Right now, safety isn’t guaranteed by the technology-it’s guaranteed by the people using it well. The data is clear: telepharmacy doesn’t sacrifice safety. It expands it. But it only works when it’s done right. And that’s the real challenge-not the tech, but the will to do it right everywhere.Is telepharmacy as safe as a regular pharmacy?
Yes, when properly implemented. Multiple studies show telepharmacy matches traditional pharmacies in dispensing accuracy (99.2-99.8%) and reduces medication errors by 15-20%. The key is strong protocols, trained staff, and reliable tech. Poor connections or rushed consultations can lower safety, but these are system failures-not inherent flaws in telepharmacy.
Can telepharmacy detect drug misuse or addiction?
It’s harder. Pharmacists rely on visual cues like sweating, shaking, or avoiding eye contact to spot potential misuse. These are harder to see on video. Some telepharmacy programs now use AI tools to flag unusual refill patterns or dosage changes, but human judgment is still critical. For high-risk patients, many programs require in-person follow-ups or partner with local clinics for physical check-ins.
Does insurance cover telepharmacy services?
Yes, under Medicare Part D since November 2022. Most private insurers now cover telepharmacy visits if they’re part of an approved health plan. Medicaid coverage varies by state, but 28 states have specific telepharmacy regulations that include reimbursement. Always check with your insurer before using the service.
What happens if the internet goes down during a telepharmacy visit?
All legitimate telepharmacy systems must have backup communication methods-like phone lines or secure text messaging. If video fails, the pharmacist should switch to audio or text to complete the consultation. Emergency situations trigger automatic alerts to local providers. Sites without backups shouldn’t be trusted. Ask your provider about their fail-safe plan before signing up.
Are telepharmacy technicians qualified to handle prescriptions?
They’re not licensed pharmacists, but they’re trained to operate dispensing machines and verify prescriptions under pharmacist supervision. The American Society of Health-System Pharmacists requires 16-24 hours of specialized training for anyone involved in telepharmacy operations. Sites with strong training programs have 22% fewer errors. Always ask if the technician is certified and if a pharmacist is reviewing every prescription in real time.
Can I still see a pharmacist in person if I use telepharmacy?
Absolutely. Most telepharmacy programs encourage in-person visits for complex cases, new diagnoses, or if you feel something isn’t right. Many rural clinics have both a telepharmacy kiosk and a visiting pharmacist on schedule. You’re not locked into remote care. Telepharmacy is designed to increase access-not replace choice.






Write a comment
Your email address will be restricted to us