When a pharmacist swaps a brand-name drug for a generic version, it’s not just a simple switch. Behind that decision is a legal, clinical, and administrative process that demands clear, accurate, and timely documentation. In the U.S., generic drugs make up nearly 90% of all prescriptions filled, saving the healthcare system billions each year. But with that efficiency comes responsibility. If the substitution isn’t properly recorded, it can lead to medication errors, insurance claim denials, or even patient harm-especially with drugs that have a narrow therapeutic index like warfarin or levothyroxine.
What Exactly Counts as a Generic Substitution?
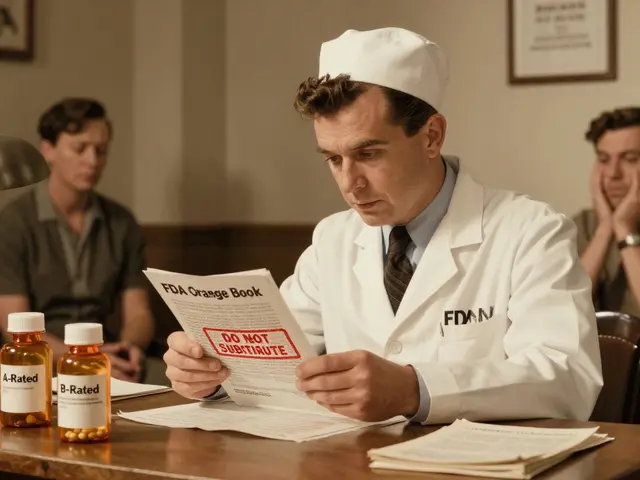
A generic substitution happens when a pharmacist dispenses a different brand or unbranded version of the drug that was prescribed-same active ingredient, same dose, same route, and proven to work the same way in the body. This isn’t random. The FDA requires generics to meet strict bioequivalence standards: their absorption rate in the bloodstream must fall within 80-125% of the brand-name drug’s levels. That’s not just a guideline-it’s a legal requirement for approval. The FDA’s Orange Book, now in its 43rd edition, is the official list of all approved generic drugs and their therapeutic equivalence ratings. Pharmacists rely on this daily to decide what can be swapped.
But here’s the catch: the FDA doesn’t control who makes the substitution. That’s left to state laws. In some places, pharmacists can swap without asking. In others, they must get the patient’s permission. And in a few, they can’t substitute at all without the prescriber’s okay. So the first rule of documentation? Know your state’s rules.
What Must Be Documented? The Core Elements
Across 48 states, pharmacists are required to record five key pieces of information every time they substitute a generic drug:
- The brand-name drug the prescriber ordered
- The generic name of the drug dispensed
- The name of the manufacturer
- The lot number
- The expiration date
This isn’t just paperwork. It’s a safety net. If a patient has a bad reaction, the pharmacist can trace the exact batch. If an insurance company denies payment, the record proves the substitution was legal. One pharmacist in Ohio told me his pharmacy lost three claims in a row because they forgot to log the manufacturer-until they added a mandatory field in their system. Now, it’s automatic.
For drugs with a narrow therapeutic index (NTI)-where even small changes in blood levels can cause harm-documentation gets stricter. Seventeen states require extra steps: notifying the prescriber, getting patient consent, and sometimes even documenting the reason why the brand was originally chosen. The American Medical Association recommends that prescribers clearly mark prescriptions as "dispense as written" when brand is medically necessary. If that note is missing, the pharmacist has to make a judgment call-and document it.
State Laws Vary-Big Time
There’s no national standard. That’s the biggest headache for pharmacists working for national chains or those who move between states.
- In 27 states, pharmacists can substitute without asking the patient.
- In 14 states, the patient must give explicit consent-verbally or in writing.
- Nine states use a hybrid model, where consent is needed only for certain drugs or patient groups.
Studies show that states requiring consent have higher prescription costs-up to $15.35 more per script in the first quarter after a brand goes generic. Why? Because patients sometimes refuse the cheaper option, even when it’s just as safe. That’s why some pharmacists now use a simple script: "This generic works the same way and costs $25 less. Would you like to switch?" That’s not just good service-it’s part of the documentation process.
Oklahoma is one of the few states that still requires prescriber authorization for any substitution. In California, starting January 1, 2024, all substitutions must be recorded in real time and made accessible to the prescriber through the electronic health record. That’s the future. Other states are catching up.
Electronic Systems Are a Must-But They’re Not Perfect
Ninety-eight percent of pharmacy chains and 87% of independent pharmacies now use electronic systems to log substitutions. That’s a huge shift from handwritten notes and paper logs. But here’s the problem: most pharmacy software wasn’t built for this.
Epic Systems, used by thousands of pharmacies, found that 32% of users needed custom tweaks just to meet their state’s documentation rules. Some systems don’t auto-populate the manufacturer name. Others don’t flag NTI drugs. One pharmacist in Texas told me her system would let her skip the lot number if she clicked "fast submit." She had to set up a mandatory pop-up warning just to stop herself from making a mistake.
Training matters. New pharmacists take 4-6 weeks to get comfortable with their state’s rules and their system’s quirks. That’s why many pharmacies now run monthly refresher sessions-not just on compliance, but on why it matters. One pharmacy in Minnesota tracked how many times they caught a potential error because someone double-checked a substitution record. They found 17 incidents in six months. None led to harm. But they could have.
Why This Matters Beyond Compliance
Good documentation isn’t just about avoiding fines. It saves lives.
A 2021 case in the Journal of the American Pharmacists Association involved a patient on warfarin. The pharmacist substituted a generic, but didn’t document the change. The patient’s INR levels spiked, leading to hospitalization. The family sued. The pharmacy lost because the record showed no indication that the substitution was reviewed for safety.
On the flip side, a 2022 study across 150 pharmacies showed that when substitution decisions were fully documented, medication errors dropped by 17.3%. Why? Because when a patient comes back with a complaint, or a doctor calls asking why the drug changed, the record tells the story. It protects the patient. It protects the pharmacist. It protects the practice.
And it’s not just about individual cases. The Congressional Budget Office estimates that if all states adopted consistent documentation standards, the healthcare system could save $4.2 billion a year by reducing adverse events tied to poor substitution records.
What’s Next? The Future of Substitution Documentation
Change is coming. The FDA’s GDUFA III rules, updated in 2022, now require manufacturers to submit more detailed bioequivalence data-especially for complex generics. That means pharmacists may soon need to document not just the drug, but why it’s equivalent.
The World Medical Association updated its stance in June 2023, urging EHR systems to include standardized fields for substitution decisions and patient outcomes. California’s real-time reporting law is already a model. Other states are watching.
Even blockchain is being tested. A pilot program by the National Pharmaceutical Council showed a 22% drop in documentation errors when substitution records were stored on a tamper-proof digital ledger. It’s still early, but it points to where this is headed: transparent, traceable, and automated.
The U.S. Department of Health and Human Services is working on national guidelines, with a draft expected in early 2024. If it passes, it could finally end the patchwork of 50 different rules. Until then, pharmacists must stay sharp-knowing their state, their system, and their patient’s needs.
How to Get It Right Every Time
Here’s a simple checklist every pharmacist should follow before hitting "dispense":
- Check the Orange Book to confirm therapeutic equivalence.
- Review the prescription for "dispense as written" or "brand necessary" flags.
- Confirm your state’s consent rules-do you need to ask the patient?
- Enter the brand name, generic name, manufacturer, lot number, and expiration date into your system.
- If it’s an NTI drug, document any prescriber notification or patient discussion.
- Complete the record within 24 hours-41 states require this.
- Double-check before closing the transaction.
It takes 30 seconds. But that 30 seconds could prevent a hospital visit.
Frequently Asked Questions
Can a pharmacist substitute a generic drug without the prescriber’s permission?
In most states, yes-unless the prescriber wrote "dispense as written" or the drug is classified as a narrow therapeutic index (NTI) medication. But state laws vary. Twenty-seven states allow pharmacists to substitute without permission, while 14 require patient consent. Oklahoma is one of the few states that still requires prescriber authorization for any substitution.
What happens if I forget to document a generic substitution?
Unrecorded substitutions can lead to insurance claim denials, legal liability, and patient safety risks. In one documented case, a patient on warfarin was hospitalized after a substitution wasn’t documented, leading to dangerous INR fluctuations. Pharmacies can face audits, fines, or even license reviews if documentation is missing or inconsistent.
Do I need to document substitutions for all generic drugs, or just certain ones?
All substitutions must be documented in 48 states. But for drugs with a narrow therapeutic index-like warfarin, levothyroxine, phenytoin, and lithium-additional steps are required in 17 states. These include notifying the prescriber, obtaining patient consent, and sometimes documenting the reason the brand was originally prescribed.
How do I know if a generic drug is therapeutically equivalent?
Use the FDA’s Orange Book (Approved Drug Products with Therapeutic Equivalence Evaluations). It lists all approved generics and assigns them a rating (like AB1, AB2) that indicates therapeutic equivalence. If a drug isn’t listed or has an RX-only rating, substitution may not be allowed without prescriber approval.
Are electronic records required for documenting substitutions?
While not federally mandated, 98% of chain pharmacies and 87% of independents use electronic systems. Many states now require electronic documentation for audit purposes, especially under Medicare Part D. Paper records are increasingly discouraged and may not meet modern compliance standards. Systems must be configured to capture all required fields, including lot number and manufacturer.
What’s the difference between bioequivalence and therapeutic equivalence?
Bioequivalence means the generic drug absorbs into the bloodstream at a rate and extent similar to the brand-within 80-125% of the original. Therapeutic equivalence means it’s not just absorbed the same way-it produces the same clinical effect and safety profile in patients. The FDA uses bioequivalence as the standard for approval, but real-world outcomes can vary slightly, especially with NTI drugs. That’s why documentation of patient response matters.
Next Steps for Pharmacists
If you’re unsure about your state’s rules, visit the National Community Pharmacists Association’s online tool-it’s updated quarterly and cross-references state laws with documentation requirements. Bookmark it. Print the checklist. Run a quick audit of your last 20 substitutions. Are all five required fields filled? Are NTI drugs flagged? Is consent documented where needed?
Don’t wait for a complaint or an audit to force you to act. Good documentation isn’t a burden-it’s your best defense. And in pharmacy practice, that’s not just professional. It’s personal.






Write a comment
Your email address will be restricted to us