When a pharmacist hands a patient a generic pill instead of the brand-name drug their doctor prescribed, it’s not just a cost-saving swap. It’s a legal act-with rules that vary by state, consequences for mistakes, and patient safety at the center. In 2023, generic medications made up 90.5% of all prescriptions filled in the U.S., yet pharmacists are the only ones who can legally make that switch. And if they get it wrong, they risk disciplinary action, lawsuits, or worse-harming a patient.
What Makes a Generic Drug Legal to Substitute?
The FDA doesn’t just approve any pill as a generic. For a drug to be considered therapeutically equivalent, it must meet strict criteria: same active ingredient, same strength, same dosage form, same route of administration, and-most critically-same bioequivalence as the brand-name version. This is tracked in the FDA Orange Book, updated monthly. Only drugs rated as ‘A’ are eligible for substitution. An ‘A’ rating means the generic performs the same in the body as the brand. An ‘B’ rating? That’s not allowed for substitution at all.
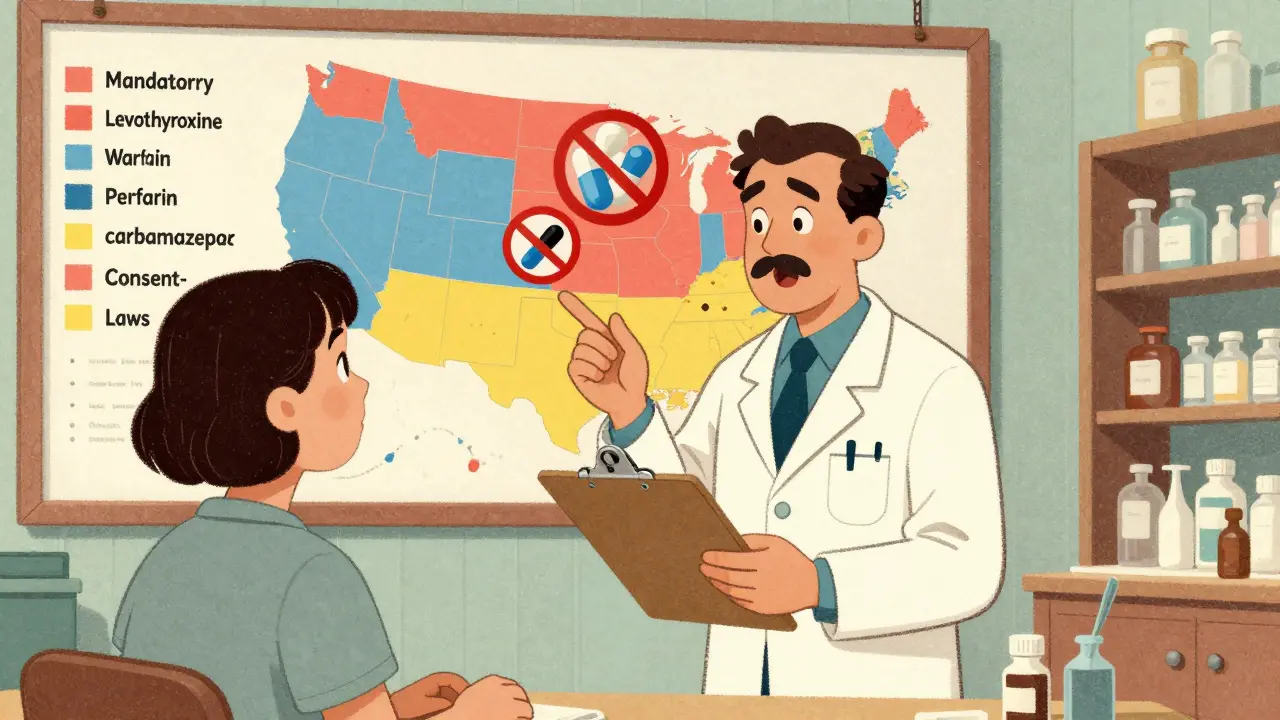
But here’s the catch: just because the FDA says two drugs are bioequivalent doesn’t mean every state lets pharmacists swap them. Some drugs, like levothyroxine for thyroid conditions or warfarin for blood thinning, have a narrow therapeutic index. That means even tiny differences in absorption can cause serious harm. The FDA says they’re safe to substitute. Some states say no-period.
State Laws Vary Wildly-Here’s What Matters
There are 51 jurisdictions in the U.S.-50 states plus D.C.-and each has its own rules. You can’t memorize them all. But you need to know the two big categories: substitution authority and consent requirements.
Mandatory substitution states-like New York, California, and Illinois-require pharmacists to substitute unless the prescriber writes ‘dispense as written’ or the patient refuses. In these states, the pharmacist has no choice. If the prescription says ‘Lisinopril’ and there’s an A-rated generic, you must dispense the generic. Failure to do so can lead to penalties.
Permissive substitution states-like Texas, Florida, and Georgia-give pharmacists discretion. You can substitute if you think it’s appropriate, but you don’t have to. That sounds flexible, but it comes with more responsibility. You’re now making a clinical judgment. And if a patient has a bad reaction, you could be held accountable.
Then there’s consent. In 18 states, substitution is assumed unless the patient objects-called presumed consent. In the other 32, you must get explicit consent before switching. That means verbal confirmation, a signed form, or an electronic acknowledgment. Skipping this step? That’s a violation-even if the drug is perfectly safe.
Drugs That Can’t Be Substituted-Even If They’re A-Rated
Some drugs are off-limits for substitution no matter what the FDA says. These aren’t random. They’re based on real-world harm.
- Antiepileptic drugs in Tennessee and Hawaii: Substitution is banned unless both the prescriber and patient give written consent. One case in 2023 involved a patient having a seizure after a pharmacist unknowingly switched their generic carbamazepine-because the pharmacy’s system didn’t flag the restriction.
- Thyroid medications in California: Even with an A rating, levothyroxine substitutions require explicit patient consent. Many patients report feeling ‘off’ after switching, even when labs show normal TSH levels.
- Anticoagulants like warfarin: Most states prohibit substitution unless the prescriber explicitly allows it. The American College of Cardiology warns that small changes in INR levels can lead to strokes or dangerous bleeding.
- Insulin and cardiac glycosides: Many states list these as ‘narrow therapeutic index’ drugs and restrict substitution. A 2019 JAMA study found a 12.7% higher rate of adverse events after switching generic digoxin.
Pharmacists who ignore these restrictions aren’t just breaking rules-they’re risking lives. State boards of pharmacy track these cases closely. In 2022, 68% of all disciplinary actions against pharmacists involved substitution errors, mostly due to documentation failures or ignoring state-specific bans.
‘Medically Necessary’ and How to Handle It
Prescribers can block substitution by writing ‘dispense as written’ or ‘medically necessary’ on the prescription. But how they do it matters. In Florida, the prescriber must write it in their own handwriting on paper prescriptions. For electronic prescriptions, they must use a specific code in the system. If they just type ‘no substitution’ in the notes field? That doesn’t count. The pharmacist must still substitute.
This creates chaos. A patient walks in with a script from a doctor who wrote ‘medically necessary’ on a printed form-but the pharmacist’s system doesn’t recognize handwritten notes. What do you do? You call the prescriber. You document the call. You don’t guess. One missed call can lead to a complaint, an audit, or worse.
Documentation Is Your Shield
Pharmacists don’t get in trouble because they made a substitution. They get in trouble because they didn’t document it.
Every time you substitute, you must record:
- The name of the generic dispensed
- The brand-name drug prescribed
- The date and time of substitution
- Whether consent was obtained and how (verbal, written, electronic)
- Any communication with the prescriber about ‘medically necessary’ flags
Electronic health record systems should auto-populate this, but they don’t always work. Many community pharmacies still use paper logs or outdated software. If you’re in a state that requires consent, and your system doesn’t prompt you for it? You still have to get it. And you still have to write it down. No shortcuts.

What Happens When You Get It Wrong?
State boards of pharmacy don’t just issue warnings. They suspend licenses. In 2022, 17 pharmacists lost their licenses nationwide for substitution violations. One in Texas substituted a generic antiepileptic for a patient with a documented seizure disorder-because the pharmacy’s system didn’t update after a state law change. The patient had a grand mal seizure. The pharmacist was charged with negligence.
Patients are also filing lawsuits. A 2023 case in Florida involved a woman who developed blood clots after switching from brand-name warfarin to a generic. Her lawyer argued the pharmacist didn’t explain the switch or get consent. The case settled for $2.1 million.
It’s not just legal risk. It’s reputational. Patients trust pharmacists to protect them. If they feel like they were switched without being told, they lose faith. A 2023 survey found that 63% of negative reviews about pharmacies cited ‘lack of notification’ as the top complaint.
How to Stay Compliant in 2026
Here’s what you need to do every day:
- Check the FDA Orange Book before dispensing any generic. Confirm the ‘A’ rating.
- Know your state’s substitution law: mandatory or permissive? Presumed or explicit consent?
- Look for ‘dispense as written’ or ‘medically necessary’ on the prescription. Don’t assume.
- Verify if the drug is on your state’s exclusion list-especially for thyroid, epilepsy, or heart meds.
- Get consent when required. Don’t rely on the patient remembering. Document it.
- Update your pharmacy’s formulary regularly. Many states require pharmacies to maintain a list of approved generics.
- Train your staff. Every new hire needs 4-6 hours of state-specific substitution training.
- Use your pharmacy software’s substitution alerts. If it doesn’t have them, push for an upgrade.
Continuing education isn’t optional. The National Community Pharmacists Association estimates pharmacists need 40-60 hours per year just to stay current on state laws. In 2022 alone, 17 states changed their substitution rules. You can’t afford to rely on memory. You need systems.
Final Thought: You’re Not Just Filling a Prescription
You’re the last line of defense between a patient and a potentially dangerous drug swap. The law gives you power-but also responsibility. The FDA says generics are safe. But the law says you have to follow your state’s rules, even when they’re stricter. And patients depend on you to know the difference.
Don’t assume. Don’t guess. Don’t skip the documentation. When it comes to generic substitution, the smallest mistake can have the biggest consequences.
Can a pharmacist substitute a generic drug without telling the patient?
Only in 18 states that allow presumed consent. In the other 32 states, pharmacists must get explicit permission from the patient before substituting. Even in presumed consent states, many pharmacists choose to inform patients anyway to avoid confusion or complaints. Failing to notify when required is a violation of state law and can lead to disciplinary action.
Are all generic drugs approved by the FDA safe to substitute?
The FDA approves generics as bioequivalent, but state laws can override that. For example, antiepileptic drugs in Tennessee and Hawaii, thyroid medications in California, and anticoagulants in many states are exempt from substitution-even if they have an ‘A’ rating in the FDA Orange Book. Pharmacists must follow state-specific restrictions, regardless of federal approval.
What happens if a pharmacist substitutes a drug that’s on a state’s exclusion list?
Substituting a drug that’s legally prohibited can result in license suspension, fines, civil lawsuits, or even criminal charges if harm occurs. In 2023, a pharmacist in Tennessee was suspended after substituting an antiepileptic drug for a patient with epilepsy. The patient suffered a seizure. State boards take these violations seriously because they directly impact patient safety.
How do pharmacists know if a prescription has a ‘medically necessary’ restriction?
It depends on the state. In Florida, the prescriber must write ‘medically necessary’ in their own handwriting on paper prescriptions. For electronic prescriptions, they must use a specific code in the system. If the restriction isn’t properly entered, the pharmacist must still substitute. Many pharmacists call the prescriber to confirm if there’s any doubt. Documentation of that call is required.
Do pharmacists need special training to dispense generics?
Yes. Most states require continuing education on substitution laws. Pharmacists should complete 40-60 hours of training annually to stay current. With 17 states changing their laws in 2022 alone, it’s not enough to rely on past knowledge. Training should cover state-specific rules, the FDA Orange Book, documentation requirements, and handling narrow therapeutic index drugs.






Write a comment
Your email address will be restricted to us