When you take cannabis with something like Xanax, Valium, opioids, or even sleeping pills, you’re not just adding two effects together-you’re multiplying the risk. The body doesn’t treat them as separate. It treats them as a team, and that team can slow your breathing to dangerous levels, make you pass out, or even stop your heart from working properly. This isn’t theoretical. Emergency rooms across the U.S. and UK are seeing more cases every year of people who woke up on the bathroom floor with no memory of how they got there, or were rushed in with oxygen levels below 85% after mixing cannabis with a prescribed depressant.
How Cannabis Acts Like a CNS Depressant
Cannabis isn’t just a relaxant-it’s a central nervous system (CNS) depressant. That means it slows down brain activity, just like alcohol, benzodiazepines, and opioids do. The main active ingredient, THC, binds to CB1 receptors in the brain, which are the same receptors involved in regulating sleep, memory, and coordination. This is why people feel calm, sleepy, or dizzy after using it. At low doses, some users report mild energy or euphoria, but even small amounts of THC-5 to 10 mg-can impair reaction time, memory, and focus in anyone, no matter how experienced they are.
When you smoke or vape cannabis, the effects hit fast-within minutes-and peak around 30 minutes. Edibles take longer: 30 to 90 minutes to start, with peak effects around 2 to 3 hours. But the high lasts longer too-up to 6 to 8 hours. That’s important because if you take a benzodiazepine at 8 p.m. and an edible at 10 p.m., you’re stacking two long-lasting depressants without realizing it.
Why the Combination Is So Dangerous
Here’s the real problem: cannabis doesn’t just add to the sedation of other depressants-it amplifies it. This is called additive sedation. When THC and a benzodiazepine like alprazolam both enhance GABA (the brain’s main calming neurotransmitter), they don’t just work side by side. They push each other harder. The result? Slowed breathing, deeper confusion, and a much higher chance of respiratory failure.
Studies show this isn’t rare. A 2020 study in the Journal of Clinical Medicine found that people using both cannabis and benzodiazepines were 3.2 times more likely to end up in the emergency room than those using benzodiazepines alone. Of those ER visits, 67% involved breathing problems. Another study from 2022 found that 38.7% of medical cannabis users were also taking prescription CNS depressants-and nearly a quarter of them had experienced a serious sedation episode that required medical help.
The risk is even higher with opioids. Both THC and opioids suppress the brainstem’s control over breathing, but through different pathways. That means the body can’t compensate the way it normally would. This is why the FDA and European Medicines Agency both issued warnings in 2022 and 2023, respectively, saying that combining cannabis with opioids can lead to death.
Real Stories, Real Consequences
On Reddit, user u/AnxietyWarrior shared: “Took half a Xanax and one hit of 20% THC flower. Woke up six hours later on the bathroom floor. No memory. Oxygen was at 82%.” That’s not an outlier. The Substance Abuse and Mental Health Services Administration (SAMHSA) recorded over 7,800 emergency visits in 2022 involving cannabis and benzodiazepines-up 42% since 2019.
Older adults are especially vulnerable. Many take opioids for chronic pain, benzodiazepines for anxiety or insomnia, and then turn to cannabis because they think it’s “natural” and safe. But aging slows how the body processes drugs. A 65-year-old using 10 mg of THC with 0.5 mg of lorazepam may experience the same level of sedation as a 25-year-old using 30 mg of THC. That’s why the American Society of Anesthesiologists recommends avoiding cannabis for at least 72 hours before surgery-because anesthetics are CNS depressants too.
What Doctors Are Doing About It
Medical professionals are catching on. The American Medical Association now advises doctors to ask every patient about cannabis use before prescribing opioids or benzodiazepines. The CDC updated its opioid guidelines in 2022 to specifically warn that cannabis can make opioids more dangerous. In California, physicians must complete a 2-hour training on cannabis-depressant interactions before they can certify patients for medical marijuana-and since that rule started in 2022, high-risk combinations have dropped by 28%.
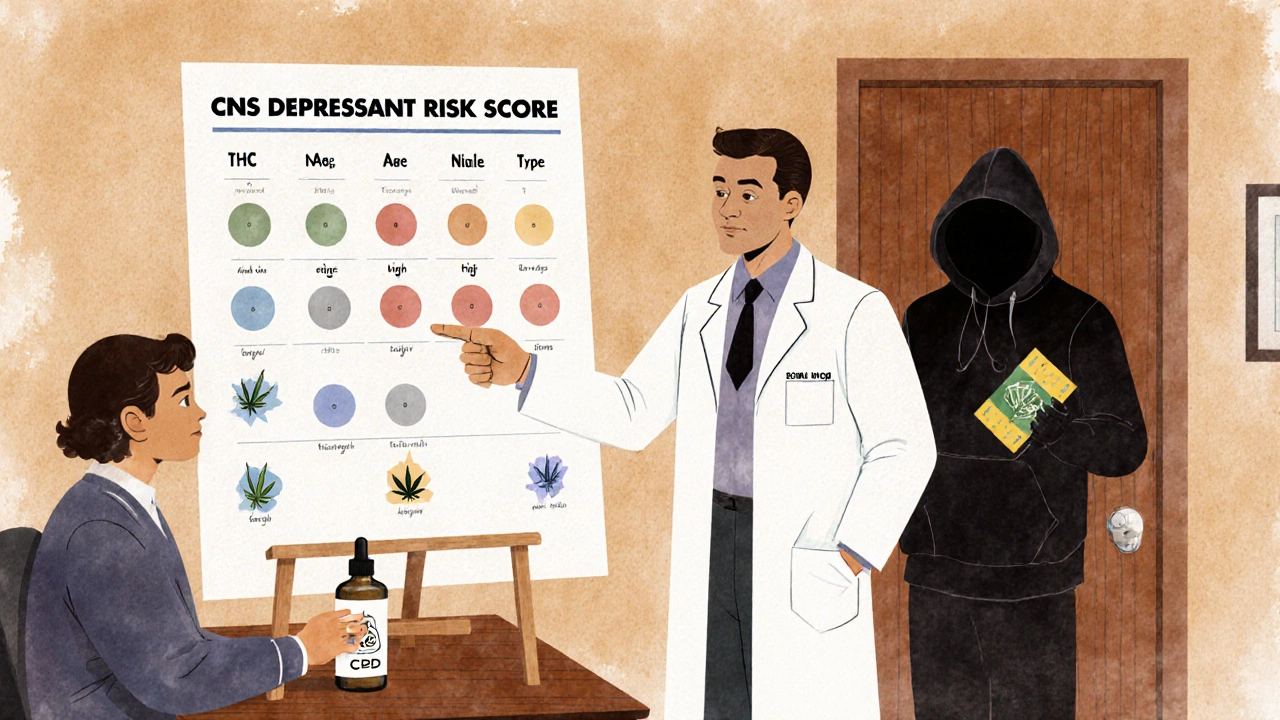
Some hospitals use a simple risk tool: score points for THC concentration (1 point for under 10%, up to 5 for over 15%), depressant type (benzodiazepines = 3, opioids = 4, barbiturates = 5), and age (2 extra points if over 65). A score above 7 means you’re at high risk and need to reconsider the combination.
Is CBD Safer?
Not all cannabis is the same. Products high in CBD and low in THC (< 0.3%) appear to carry much lower risk. A 2022 double-blind trial in JAMA Internal Medicine gave 127 people 150 mg of CBD oil daily with alprazolam. No significant interaction was found. CBD doesn’t bind strongly to CB1 receptors like THC does, so it doesn’t cause the same level of sedation or cognitive impairment. That’s why some patients with epilepsy or chronic pain are switching to CBD-dominant products under medical supervision.
But don’t assume all CBD products are safe. Many are poorly regulated. A 2023 study found that nearly 30% of CBD oils sold online contained more THC than labeled-sometimes enough to cause sedation on its own. Always check third-party lab reports and avoid anything with unknown potency.
How to Reduce Risk If You’re Using Both
If you’re prescribed a CNS depressant and use cannabis, here’s what you can do:
- Avoid mixing them entirely. The safest choice is to use one or the other-not both.
- If you must use both, keep THC low. Stick to products under 5% THC. Avoid edibles and concentrates.
- Space out doses. Wait at least 4 hours between taking a depressant and using cannabis. Never use them at the same time.
- Never drive or operate machinery. Even if you feel fine, your reaction time is impaired.
- Tell your doctor. Don’t hide your cannabis use. They need to know to adjust your medications safely.
- Watch for warning signs. If you feel extremely drowsy, confused, have trouble breathing, or can’t remember things clearly-seek help immediately.
What’s Next?
Research is moving fast. The National Institutes of Health spent over $140 million in 2023 studying cannabis-drug interactions, up from less than $30 million in 2020. Scientists are now working on standardized risk scores and safe THC thresholds for each type of depressant. The American College of Physicians wants all states with medical cannabis programs to require interaction screening by 2025-something that could prevent over 2,300 ER visits a year.
For now, the message is clear: combining cannabis with CNS depressants isn’t a gray area. It’s a red flag. Whether you’re using it for pain, anxiety, or sleep, the cost of mixing it with other sedatives can be your life.
Can I use CBD with benzodiazepines safely?
CBD-dominant products with very low THC (<0.3%) appear to have minimal interaction with benzodiazepines based on current research. A 2022 study found no significant increase in sedation or respiratory risk when high-CBD oil was taken with alprazolam. However, many CBD products on the market contain hidden THC or inconsistent dosing. Always choose third-party tested products and consult your doctor before combining them with any prescription medication.
How long should I wait after using cannabis before taking a depressant?
Wait at least 4 hours after using cannabis before taking a CNS depressant like a benzodiazepine or opioid. This is especially important if you’ve used an edible, since effects can last 6-8 hours. Even if you feel “over it,” your body is still processing THC. Slowing down your breathing and reaction time can still be happening without you noticing. When in doubt, wait longer.
Is it safe to use cannabis after surgery?
No. Anesthesiologists recommend avoiding cannabis for at least 72 hours before and after surgery. Cannabis can interfere with how anesthetics work, requiring higher doses to achieve sedation-and increasing the risk of breathing problems during recovery. Patients who use cannabis regularly often need more pain medication post-op and are more likely to experience complications like low oxygen levels or prolonged sedation.
Can cannabis help reduce opioid use?
Some studies show that low-dose THC (2.5-5 mg) under strict medical supervision can help certain chronic pain patients reduce opioid use by nearly half. But this only works in controlled settings with regular monitoring. It does not mean you can safely replace opioids with cannabis on your own. Combining the two without oversight increases overdose risk. Never adjust your opioid dose without talking to your doctor.
Why do some people feel energized after using cannabis?
At very low doses, especially with sativa-dominant strains, some people experience mild stimulation-increased heart rate, alertness, or euphoria. But this doesn’t mean cannabis isn’t a depressant. The same person can feel energized one time and sedated another, depending on dose, tolerance, and environment. Even in these cases, cognitive and motor skills are still impaired. The depressant effects become clear when combined with other sedatives, regardless of how you initially felt.
Are there any legal protections if I’m prescribed both?
No. Even in places where cannabis is legal, combining it with prescription depressants can violate your medication agreement or insurance policy. Doctors are legally required to warn you about the risks, and pharmacists may refuse to fill prescriptions if they know you’re using both. In emergencies, hospitals will treat you regardless, but they may report unsafe use to your provider or state board. The safest path is to avoid the combination entirely.
Final Takeaway
Cannabis and CNS depressants don’t play nice together. The risks aren’t just about feeling sleepy-they’re about stopping your breathing, losing memory, or ending up in the hospital. If you’re using either one, talk to your doctor before adding the other. There’s no safe middle ground when your life is on the line. Better to find another way to manage your symptoms than to gamble with something that’s already killing people.






Write a comment
Your email address will be restricted to us