What Exactly Is a Drug Allergy?
A drug allergy isn’t just a side effect. It’s your immune system overreacting to a medication, treating it like an invader. That’s why one person can take penicillin with no issues, while another breaks out in hives or struggles to breathe. The difference? Immune system involvement. According to the National Institutes of Health, true drug allergies are actually uncommon - but they’re often misdiagnosed. Around 10% of people in the U.S. say they’re allergic to a drug, but more than 90% of those labeled as penicillin-allergic turn out to be fine after proper testing.
Common Signs of a Drug Allergy
The most obvious sign? A rash. But not all rashes are the same. Here’s what to look for:
- Hives - raised, red, itchy welts that can show up anywhere on the skin. They may come and go within hours.
- Itching - intense, widespread itching without a visible rash. This can be the first clue.
- Swelling - especially around the lips, tongue, eyes, or throat. This is serious if it affects breathing.
- Difficulty breathing - wheezing, tightness in the chest, or feeling like you can’t get air in. This isn’t just a cold - it’s your airways reacting.
- Fever, joint pain, swollen lymph nodes - these show up days or weeks after taking the drug, often with a rash. This could be serum sickness or DRESS syndrome.
- Blisters or peeling skin - if your skin starts blistering, peeling, or forming target-shaped lesions, especially around the mouth or eyes, this could be Stevens-Johnson Syndrome or Toxic Epidermal Necrolysis. These are medical emergencies.
Timing matters. If symptoms hit within an hour of taking a pill or getting an injection, it’s likely an IgE-mediated reaction - the kind that can lead to anaphylaxis. But rashes from drugs like amoxicillin or sulfa drugs can show up days or even weeks later. Don’t assume it’s just a virus if you feel off a week after starting a new medication.
When It’s an Emergency: Anaphylaxis
Anaphylaxis isn’t just a bad reaction - it’s life-threatening. It happens when your immune system releases a flood of chemicals that crash your blood pressure and shut down your airways. The key sign? It affects two or more body systems at once.
For example:
- A rash and trouble breathing
- Swelling and vomiting or diarrhea
- Feeling dizzy and your skin turning pale or blue
If you or someone else has these signs, call 911 immediately. Don’t wait. Don’t try to drive yourself. Anaphylaxis can kill in minutes. If you have an epinephrine auto-injector (like an EpiPen), use it right away - even if you’re not sure. Better to use it and be fine than to wait and risk losing time.
Delayed Reactions You Can’t Ignore
Not all drug allergies show up fast. Some sneak in slowly, making them easy to miss.
Serum sickness-like reactions show up one to three weeks after starting a drug. You’ll get a rash, fever, swollen joints, and swollen glands. It feels like the flu, but it’s your body attacking the medication.
DRESS syndrome (Drug Reaction with Eosinophilia and Systemic Symptoms) is rarer but more dangerous. It can cause liver damage, kidney problems, and high white blood cell counts. Symptoms include a widespread rash, fever, swollen lymph nodes, and sometimes jaundice. If you’ve been on antibiotics like minocycline, anticonvulsants like carbamazepine, or allopurinol for a few weeks and suddenly feel awful, get checked.
Stevens-Johnson Syndrome (SJS) and Toxic Epidermal Necrolysis (TEN) are extreme forms. Skin starts to blister and peel off in sheets. Mucous membranes in your mouth, eyes, or genitals break down. This isn’t a rash - it’s like a severe burn from the inside out. Survival depends on getting to a burn unit fast.
How Doctors Diagnose Drug Allergies
There’s no single blood test for most drug allergies. Diagnosis comes down to your story - when you took the drug, what happened, how fast it came on, and what it looked like.
For penicillin, there’s a reliable test: skin prick tests. A tiny amount of penicillin is placed under your skin. If you’re allergic, a red, itchy bump appears. If that’s negative, you might get an oral challenge - swallowing a small dose under medical supervision. If nothing happens, you’re not allergic. Many people are mislabeled because they had a rash as a child and were told never to take penicillin again. But most of them can take it safely now.
For other drugs, like sulfa or NSAIDs, testing is limited. Blood tests can help in cases of DRESS or severe delayed reactions, but they’re not foolproof. Your doctor will rely on your history, physical exam, and sometimes a photo of the rash. If you’re not sure what you’re reacting to, take pictures the next time you get a rash after taking a new drug. That visual record helps.
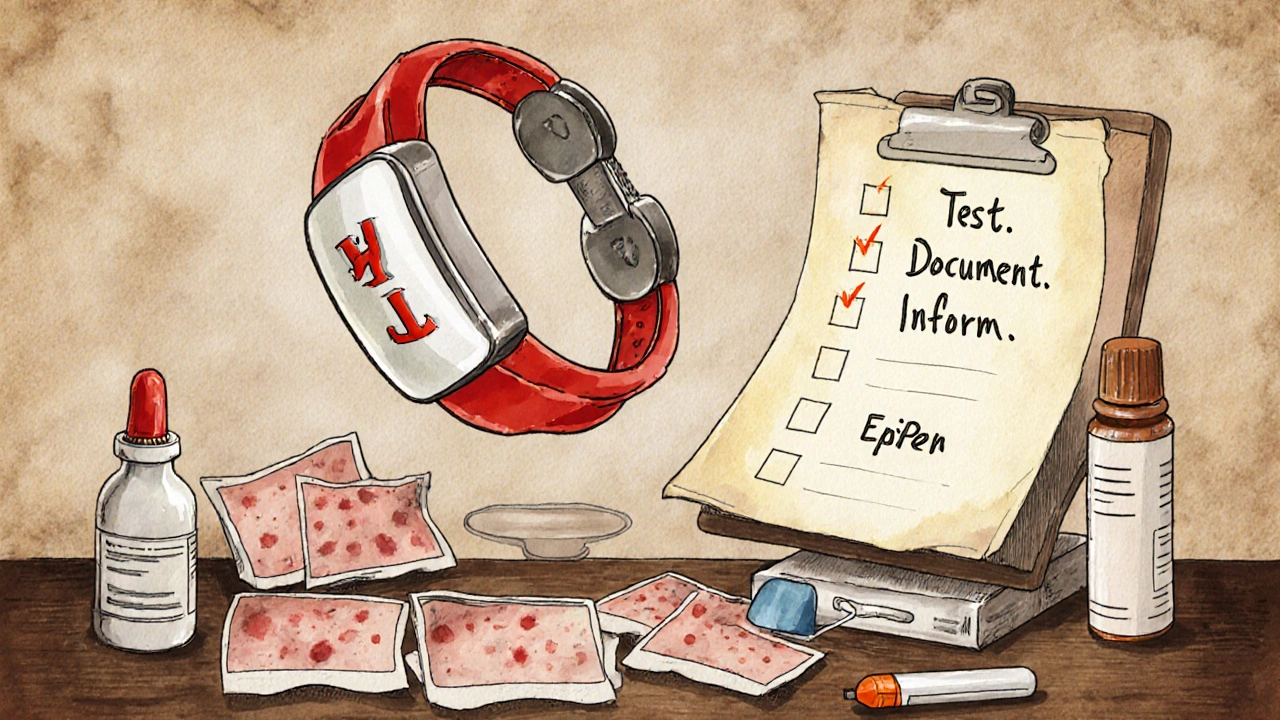
What to Do After a Reaction
Stop the drug. That’s step one. But don’t just stop and assume it’s fine. Here’s what to do next:
- Write it down. Name the drug, dose, when you took it, and exactly what happened - symptoms, timing, how long it lasted.
- Take photos. Rashes change fast. A picture from day one helps your doctor spot patterns.
- See your doctor. Don’t wait for the next scheduled appointment. Call and say you had a possible allergic reaction. They’ll refer you to an allergist if needed.
- Get tested. Especially if it’s penicillin or another common drug you might need again. Testing can remove a lifetime of unnecessary restrictions.
- Update your records. Make sure your primary care doctor, pharmacist, and hospital records reflect the correct diagnosis. Many people are wrongly labeled in electronic systems, leading to worse treatments later.
Why Mislabeling Is Dangerous
Being labeled “allergic to penicillin” sounds harmless - until you get pneumonia, a serious infection, or need surgery. Then doctors reach for broader-spectrum antibiotics like vancomycin or ciprofloxacin. These are more expensive, harder on your gut, and increase your risk of deadly infections like C. diff.
Studies show that people wrongly labeled as penicillin-allergic have longer hospital stays, higher costs, and more complications. That’s why the NIH calls accurate diagnosis a public health goal. If you think you’re allergic to a common drug, get it checked. You might be able to use safer, cheaper, more effective treatments.
What You Can Do Now
If you’ve ever had a rash, swelling, or breathing trouble after a medication:
- Don’t assume it’s just “something you’re sensitive to.”
- Don’t avoid all antibiotics because of one bad reaction.
- Don’t wait until you’re sick again to figure it out.
Take action. Write down your reaction. Talk to your doctor. Ask about an allergist referral. If you’re in the UK, your GP can refer you to a specialist. You don’t need to live with a label that might be wrong - and could be putting your health at risk.
Preventing Future Reactions
Once you know what you’re allergic to:
- Wear a medical alert bracelet.
- Keep a list of safe and unsafe drugs in your phone and wallet.
- Always tell every doctor, dentist, and pharmacist about your reaction - even if it was years ago.
- Ask: “Is there an alternative that doesn’t carry this risk?”
Most importantly - don’t let fear stop you from getting care. Many drug allergies can be safely ruled out. And if you truly have one, knowing it means you can avoid dangerous mistakes in the future.
Can a drug allergy develop after taking a medication for years?
Yes. Drug allergies can develop at any time, even after years of safe use. Your immune system can suddenly start reacting to a drug you’ve taken before without issue. This is common with antibiotics like penicillin, painkillers like ibuprofen, or seizure medications. If you notice new symptoms - rash, swelling, trouble breathing - after taking a long-used drug, stop it and see a doctor.
Are over-the-counter drugs like ibuprofen or aspirin common causes of allergies?
Yes. NSAIDs like ibuprofen and aspirin can cause allergic-like reactions, though they’re not always true IgE-mediated allergies. Symptoms include hives, asthma flare-ups, or nasal congestion. People with chronic hives or asthma are more likely to react. If you’ve ever had a reaction to these, avoid them unless tested by an allergist.
Can I outgrow a drug allergy?
Yes, especially with penicillin. Studies show that 80% of people who had a penicillin allergy in childhood lose it within 10 years. But you can’t assume it’s gone - you need proper testing to confirm. Never try to take the drug again on your own. Testing is safe and done under medical supervision.
If I’m allergic to penicillin, am I allergic to all antibiotics?
No. Penicillin belongs to the beta-lactam family, but not all antibiotics are related. Cephalosporins, macrolides like azithromycin, and tetracyclines are different classes. Most people with penicillin allergy can safely take these. Only about 1 in 10 will react to cephalosporins, and even then, it’s usually mild. An allergist can help determine which antibiotics are safe for you.
Should I carry an epinephrine auto-injector if I have a drug allergy?
Only if you’ve had a previous anaphylactic reaction to a drug, or if your allergist recommends it. If your reaction was only a rash or mild swelling, you likely don’t need one. But if you’ve ever had trouble breathing, low blood pressure, or swelling of the throat, carrying an EpiPen could save your life. Talk to your allergist about your risk level.







Write a comment
Your email address will be restricted to us