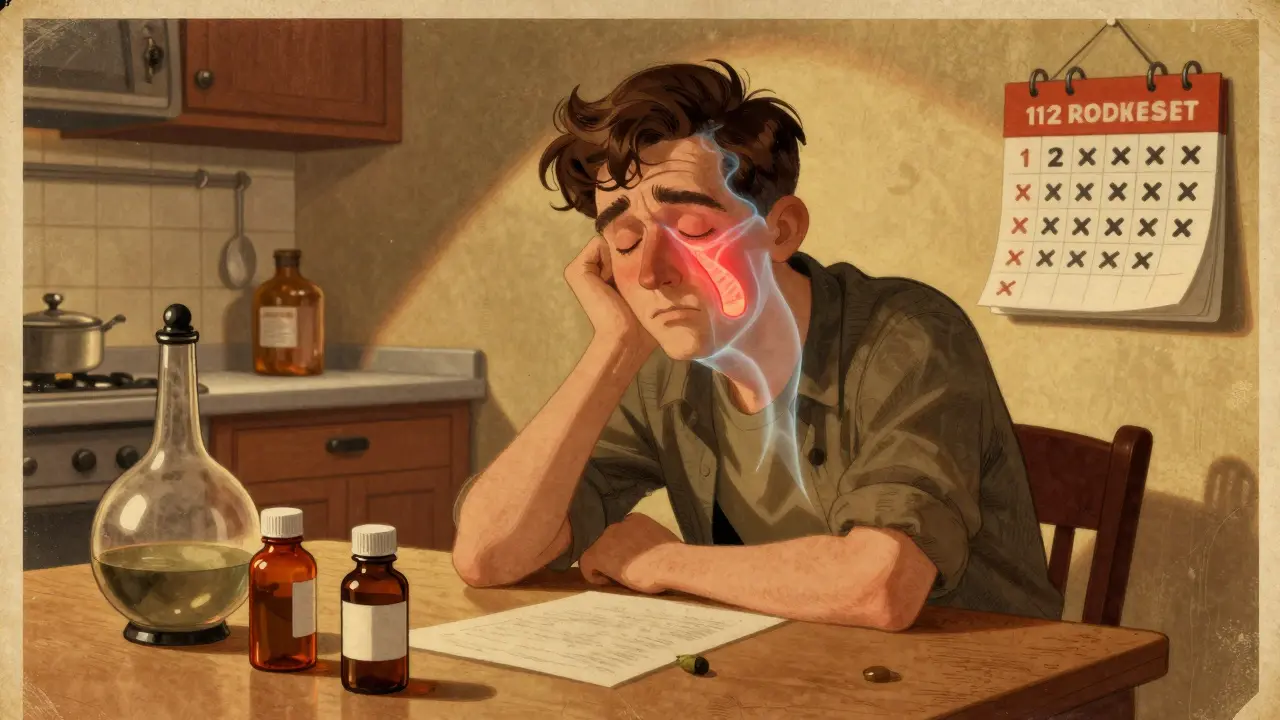
When your nose stays blocked for months - even after trying decongestants, antibiotics, or steam inhalation - it’s not just a bad cold. It could be chronic sinusitis, a condition that affects nearly 1 in 10 people worldwide. Unlike acute sinusitis that clears up in a few weeks, chronic sinusitis lingers for 12 weeks or longer, no matter what you do. It doesn’t just make you feel tired. It steals your sleep, your sense of smell, and sometimes even your mood. And the truth? Most people don’t realize it’s not just an infection. It’s inflammation - often triggered by allergies, structural issues, or both.
What Exactly Is Chronic Sinusitis?
Chronic sinusitis, also called chronic rhinosinusitis, isn’t one single problem. It’s a group of conditions where the lining of your sinuses - the hollow spaces behind your forehead, cheeks, and nose - becomes swollen and inflamed for months. This swelling blocks the tiny drainage channels, trapping mucus inside. That trapped mucus becomes a breeding ground for bacteria, but here’s the catch: most cases aren’t caused by active infection. Instead, it’s your body’s own immune response gone haywire.
The European Position Paper on Rhinosinusitis and Nasal Polyps (EPOS) 2020 defines it clearly: you have chronic sinusitis if you’ve had at least two of these symptoms for 12+ weeks:
- Nasal blockage or congestion
- Thick nasal discharge (clear or yellow-green)
- Facial pain or pressure - especially around your eyes, cheeks, or forehead
- Reduced or lost sense of smell
Doctors confirm this with a nasal endoscopy - a thin, flexible camera inserted into the nose - or a CT scan that shows swollen tissue or fluid buildup. If you’ve been told you have "sinusitis" for years and nothing worked, this is likely what you’ve been dealing with.
The Three Main Types: Allergies, Polyps, and Inflammation
Not all chronic sinusitis is the same. There are three major subtypes, and knowing which one you have changes everything about your treatment.
1. Chronic sinusitis without nasal polyps - This is the most common form. It’s often linked to ongoing inflammation from environmental irritants like cigarette smoke, pollution, or dry air. People with asthma are 3 to 4 times more likely to develop this type because the same inflammatory pathways affect both the lungs and sinuses.
2. Chronic sinusitis with nasal polyps - About 1 in 4 people with chronic sinusitis have these soft, grape-like growths inside the nasal passages. They’re not cancerous, but they can grow large enough to block airflow and smell. These are strongly tied to allergies, especially in people with Samter’s triad: asthma, nasal polyps, and aspirin sensitivity. If you’ve tried nasal sprays and still can’t breathe, polyps might be the culprit.
3. Allergic fungal rhinosinusitis - Less common but more complex. This happens when your immune system overreacts to harmless fungi in the air. It’s not an infection like a cold - it’s an allergic response to mold spores. You might have thick, sticky mucus that looks like toothpaste, and your symptoms often worsen in damp weather.
Doctors use endoscopy and CT scans to tell these apart. If you have polyps or fungal material, your treatment path changes dramatically.
Why Antibiotics Usually Don’t Work
Many people expect antibiotics to fix chronic sinusitis. After all, if your nose is full of gunk, it must be infected, right? Not so fast.
Research from the National Center for Biotechnology Information (NCBI) shows that 70% of chronic sinusitis cases have no active bacterial infection. The bacteria present - like Streptococcus pneumoniae or Haemophilus influenzae - are just living there, not causing harm. Giving antibiotics in these cases doesn’t help, and it can lead to side effects like diarrhea or yeast infections.
The American Academy of Allergy, Asthma & Immunology (AAAAI) says it plainly: "Treating chronic sinusitis with antibiotics usually doesn’t help." Antibiotics are only useful if you have a sudden flare-up - like a bacterial infection on top of your chronic condition - which happens in maybe 10-15% of cases.
That’s why so many people feel frustrated. They’ve been prescribed antibiotics three or four times, and nothing changed. That’s not their fault. It’s just the wrong tool for the job.

The First-Line Treatment: Saline and Steroids
If antibiotics won’t fix it, what will? The answer is simple, cheap, and backed by solid evidence: daily nasal saline irrigation and intranasal corticosteroid sprays.
Nasal saline irrigation - using a neti pot or squeeze bottle with sterile saltwater - flushes out allergens, mucus, and irritants. Studies show it improves symptoms in over 80% of people within 4 to 8 weeks when used daily.
Then comes the steroid spray. These aren’t the same as bodybuilding steroids. They’re anti-inflammatory drugs that target the nasal lining directly. Common ones include:
- Fluticasone (Flonase)
- Budesonide (Rhinocort)
- Mometasone (Nasonex)
- Beclomethasone (Beconase)
Mayo Clinic data shows these reduce inflammation in 60-70% of patients. But here’s the catch: you have to use them every day, for at least 8 weeks. Most people stop after a few days because they don’t feel instant relief. That’s why only about 60% stick with them long-term.
For allergy-driven cases, antihistamines like loratadine (Claritin) or cetirizine (Zyrtec) help too. They reduce sneezing and runny nose, but they don’t fix the swelling. That’s why they’re used alongside sprays - not instead of them.
When Medication Fails: Biologics and the New Frontier
What if you’ve tried everything - saline, sprays, antihistamines - and you’re still struggling to breathe or smell? That’s when biologic therapies come in.
In 2019, the FDA approved dupilumab (Dupixent) specifically for chronic sinusitis with nasal polyps. This is a monoclonal antibody injected under the skin every two weeks. It blocks key inflammation signals in the body. In clinical trials, patients saw:
- 50-60% reduction in polyp size
- 30-40% improvement in nasal congestion
- Up to 70% improvement in sense of smell
Other biologics like omalizumab (Xolair) and mepolizumab (Nucala) are also used, especially for people with asthma or allergies. Colorado ENT reports 35-55% symptom improvement in treatment-resistant cases.
These aren’t cheap - they cost thousands per year - but for people who can’t breathe, sleep, or work because of polyps, they’re life-changing. They’re now being used in the UK’s NHS for severe cases that don’t respond to steroids.
Surgery: What Really Works
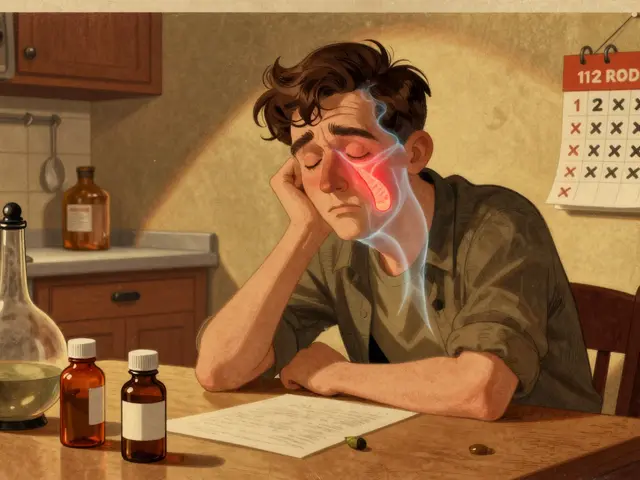
Surgery isn’t the first option. But if you’ve tried 12 weeks of medical treatment and still can’t function, it’s time to consider it.
The gold standard is Functional Endoscopic Sinus Surgery (FESS). It’s not open surgery. It’s done through the nose using a tiny camera and instruments. The surgeon clears blocked passages, removes polyps, and widens drainage routes. Success rates? 75-90% of patients report major improvement. Recovery takes about a week.
A less invasive option is balloon sinuplasty. A small balloon is inflated inside the blocked sinus to stretch it open. It’s quicker - recovery in 3-5 days - and has fewer risks. But studies from Mayo Clinic show it’s less effective long-term, especially for people with large polyps or severe inflammation.
If you have a deviated septum - a crooked wall between your nostrils - your surgeon might combine FESS with a septoplasty. Cleveland Clinic data shows 65-75% of these patients get lasting relief.
For nasal polyps, a simple polypectomy (removing the polyps) gives quick relief - 85% of patients feel better right away. But here’s the reality: without ongoing steroid sprays, polyps come back in 40-50% of cases within 18 months.

Lifestyle Changes That Actually Help
Medication and surgery help - but if you don’t change your environment, symptoms will keep coming back.
- Use a humidifier - Dry air dries out your nasal lining. Adding moisture (especially in winter) cuts congestion by 40% in many people.
- Avoid smoke and strong fumes - Tobacco smoke increases risk by 35%. Even secondhand smoke or cleaning chemicals can trigger flares.
- Wash your bedding weekly - Dust mites are a major allergen. Use hypoallergenic pillowcases and wash sheets in hot water.
- Stay hydrated - Thin mucus drains better. Aim for 2 liters of water daily.
- Check your air filter - A good HEPA filter in your bedroom can reduce airborne allergens by up to 60%.
For those with Samter’s triad (asthma + polyps + aspirin sensitivity), aspirin desensitization under medical supervision improves symptoms in 70-80% of cases. It’s not for everyone, but it’s a game-changer for those who qualify.
What Happens If You Do Nothing?
Chronic sinusitis isn’t just annoying. Left untreated, it can lead to complications - though they’re rare.
Cleveland Clinic reports that fewer than 0.5% of people develop serious issues like:
- Infection spreading to the eye socket (orbital cellulitis)
- Bone infection (osteomyelitis)
- Brain infection (meningitis or abscess)
These are emergencies. But more commonly, untreated sinusitis leads to:
- Chronic fatigue
- Sleep apnea from nasal blockage
- Loss of smell (which can lead to depression or loss of appetite)
- Difficulty concentrating at work or school
The real cost? Your quality of life. Mayo Clinic found that 65% of patients say their symptoms interfere with daily tasks - cooking, working, even socializing.
When to See a Specialist
If you’ve had symptoms for 12 weeks or more - and over-the-counter remedies haven’t helped - it’s time to see an ENT (ear, nose, and throat) doctor. Don’t wait until you’re desperate.
You should also seek help if:
- You’ve had multiple courses of antibiotics with no improvement
- You’ve lost your sense of smell
- You have asthma or allergies and your nose symptoms are worsening
- You notice swelling around your eyes or forehead
A good ENT will do more than just look in your nose. They’ll review your history, order imaging if needed, and consider whether allergies, polyps, or structural issues are the real problem. They might even refer you to an allergist or immunologist for testing.
Can chronic sinusitis be cured?
Chronic sinusitis can be managed very effectively - but "cured" isn’t the right word. It’s a long-term condition, like asthma or high blood pressure. With the right combination of nasal sprays, saline rinses, and lifestyle changes, most people can live symptom-free. Surgery and biologics can provide long-lasting relief, but ongoing maintenance is usually needed to prevent recurrence.
Are nasal steroid sprays safe for long-term use?
Yes. Unlike oral steroids, nasal sprays deliver a tiny amount of medication directly to the nasal lining. Less than 1% enters your bloodstream. Long-term use (even years) is considered safe by the American Academy of Otolaryngology. Side effects like nosebleeds or dryness are mild and usually go away with proper technique. Always use the spray aimed away from the nasal septum to avoid irritation.
Do I need a CT scan to diagnose chronic sinusitis?
Not always. If your symptoms are clear and you respond to treatment, a scan isn’t needed. But if your symptoms are severe, persistent, or don’t improve with standard treatment, a CT scan helps identify polyps, structural issues, or fungal involvement. It’s especially useful before surgery.
Why do some people get chronic sinusitis and others don’t?
It’s a mix of genetics, environment, and immune response. People with asthma, allergies, or a family history are more likely. Environmental factors like pollution, smoking, or dry air also play a big role. Some people have naturally narrower sinus passages, making them more prone to blockage. It’s not about being "dirty" - it’s about how your body reacts to everyday triggers.
Is surgery worth it if polyps keep coming back?
Yes - if you combine it with ongoing medical treatment. Surgery removes the blockage and gives you breathing room. But if you stop using nasal steroids after surgery, polyps will likely return. The goal isn’t one-time fix - it’s long-term control. Many patients find that after surgery, they need less medication and feel much better than before.
If you’ve been living with blocked sinuses for months, you’re not alone. And you don’t have to keep suffering. The tools to manage it - from saline rinses to biologics - are more effective than ever. The key is matching the treatment to the cause. Don’t guess. Get tested. Get the right care. And breathe easier again.



Write a comment
Your email address will be restricted to us