When your stomach suddenly locks up in sharp, unrelenting pain-right under your ribs, sometimes radiating to your back or shoulder-you might think it’s indigestion. But if it happens again and again, especially after fatty meals, it’s probably not just a bad taco. It could be gallstones. And if left untreated, those tiny stones can turn a bad night into a hospital trip, or worse.
What Happens When Gallstones Block the Flow
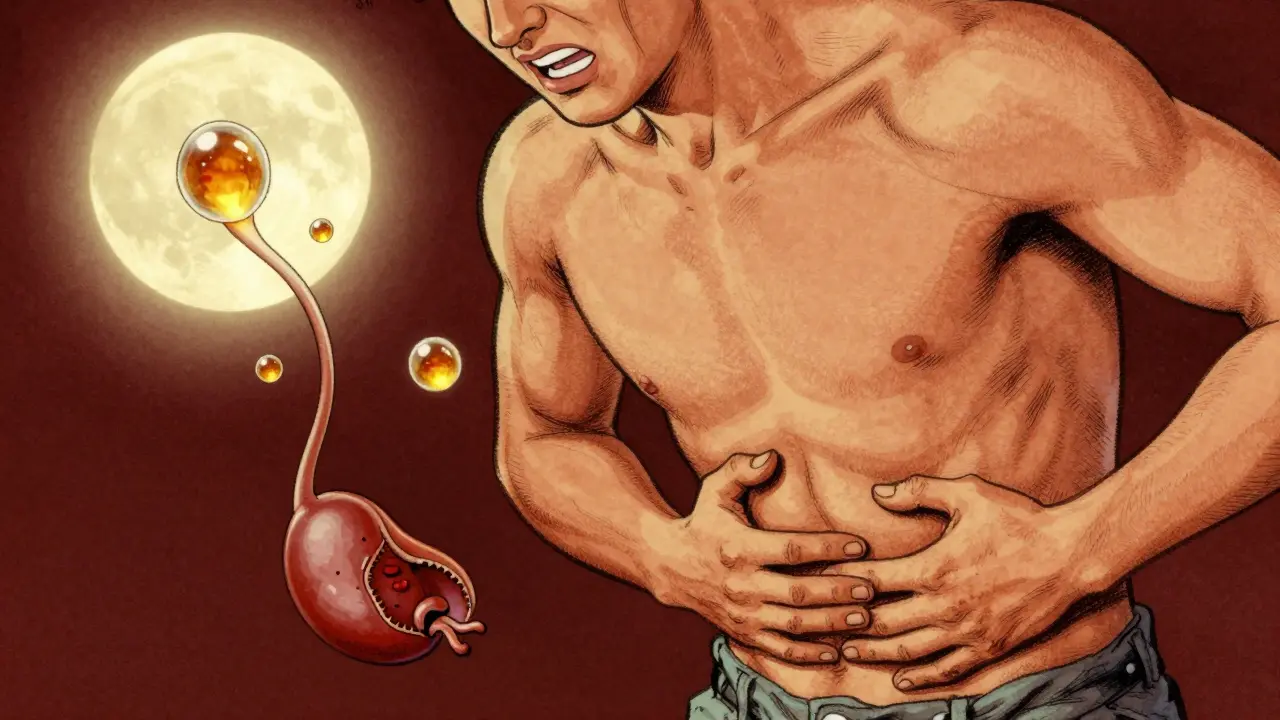
Gallstones are hardened deposits of bile, mostly made of cholesterol (80% of cases in the UK and US), or bilirubin (the rest). They form when your gallbladder doesn’t empty properly or when bile becomes too concentrated. Most people have them and never know-about 80% of those with gallstones never have symptoms. But for the other 20%, things get serious fast.
The first warning sign is biliary colic. This isn’t a dull ache. It’s a sudden, steady, moderate-to-severe pain that hits like a hammer in the upper right side of your belly or just below your breastbone. It doesn’t come and go like gas. It starts abruptly, peaks within an hour, and lasts 1 to 5 hours. You can’t burp it out. You can’t poop it out. Vomiting doesn’t help. It’s caused by a stone temporarily blocking the cystic duct-the pipe that lets bile leave your gallbladder. When the stone moves, the pain fades. But it will come back. And it usually does.
According to the American Academy of Family Physicians, more than 90% of people who’ve had one episode of biliary colic will have another within 10 years. Two-thirds will have a repeat within just two years. That’s not a coincidence. It’s a pattern. And each episode increases your risk of something worse.
When Biliary Colic Turns Into Cholecystitis
If a stone stays stuck for more than a few hours, your gallbladder starts to swell and inflame. That’s acute cholecystitis. It’s no longer just pain-it’s fever, nausea, vomiting, and tenderness so bad you can’t even take a deep breath without it hurting. Your skin might turn yellow (jaundice) if the stone moves into the main bile duct. That’s choledocholithiasis. Or worse, it can trigger pancreatitis.
One in five people who get biliary colic will develop cholecystitis. And if you end up in the ER with it, the clock starts ticking. The Society of American Gastrointestinal and Endoscopic Surgeons says surgery should happen within 72 hours. Delay it, and the chance your surgeon has to switch from a minimally invasive laparoscopic procedure to a large open cut increases from 7% to 25%. That means longer recovery, more pain, and higher risk of infection.
Studies show untreated symptomatic gallstones lead to emergency hospitalization in 20-30% of cases within five years. That’s not a small risk. It’s a guarantee that something bad will happen if you wait.
The Gold Standard: Laparoscopic Cholecystectomy
There’s only one treatment that reliably stops this cycle: removing the gallbladder. Not the stones. The whole organ. Why? Because as long as you have a gallbladder, it can make more stones. And if it’s already inflamed, it’s not working right anyway.
Laparoscopic cholecystectomy is the standard. It’s done through four tiny cuts in your abdomen. A camera and tools go in. The gallbladder is clipped, cut, and removed. Most patients go home the same day or the next. Recovery? About a week. Compare that to open surgery-where they cut through your whole abdomen-which takes 4-6 weeks to recover from.
Nearly 90% of gallbladder removals in the UK and US today are laparoscopic. Success rates? Over 95%. Complication rates? Below 2% in experienced hands. Patients report massive improvements in quality of life. One woman in Cleveland Clinic’s 2023 case study had 17 episodes over 18 months. After surgery, her pain vanished in 10 days. She was back to full activity in two weeks.
But it’s not perfect. About 12% of people get diarrhea after surgery. That’s because bile flows directly into the intestine now, without being stored. For most, it settles down in a few months. A smaller group-around 6%-get post-cholecystectomy syndrome: ongoing pain, bloating, or nausea. Sometimes it’s due to leftover stones, sometimes it’s functional gut issues. It’s rare, but real.
What About Nonsurgical Options?
You might hear about pills that dissolve gallstones. Ursodeoxycholic acid can work-but only for small, pure cholesterol stones, and only if your gallbladder still works well. Even then, it takes 6 to 24 months. And even if it works, half the people get stones back within five years. It’s not a cure. It’s a temporary fix.
Shockwave therapy to break up stones? Used to be popular. Now? Almost never done. The stones break, but they often re-form. Plus, you still need to take pills for months. The risk-benefit doesn’t add up.
There’s a new option for high-risk patients: endoscopic ultrasound-guided gallbladder drainage. It’s not a cure, but it’s a bridge. For someone too sick for surgery, this drains the gallbladder through a tiny tube placed via the stomach. It’s 85% effective at relieving infection and buying time. But it’s not a replacement for removal. Just a way to survive until you’re strong enough for the real fix.
Who Shouldn’t Have Surgery?
Not everyone needs an operation. For healthy people under 75 with symptoms? Surgery is the clear choice. But for older adults, especially over 75 with heart disease, diabetes, or lung problems? The risks climb. The 30-day death rate after gallbladder surgery jumps from 0.1% in healthy patients to 2.8% in those with three or more serious conditions.
That doesn’t mean no surgery. It means careful planning. A 78-year-old with frequent attacks and a strong heart might still benefit. A 90-year-old with advanced dementia and no quality of life to regain? Probably not. Doctors now use better tools to weigh risk versus benefit. It’s not about age-it’s about health, function, and what matters to the patient.

What Patients Say: Real Stories, Real Pain
On patient forums, the same themes repeat. People describe waiting months-sometimes years-to get diagnosed. One person saw five doctors before an ultrasound found the stones. Another said they were told it was ‘just stress’ until they collapsed in the ER.
Those who waited too long often say they wish they’d acted sooner. One Reddit user wrote: ‘I thought I’d tough it out. I didn’t realize how much I was missing-eating with my family, sleeping through the night, walking without pain.’
Another common complaint? Poor pain control in the ER. NSAIDs like ketorolac work as well as opioids for biliary colic, but with fewer side effects. Yet many hospitals still default to strong narcotics. That’s changing, but slowly.
What’s Next for Gallstone Treatment?
Research is pushing forward. Enhanced Recovery After Surgery (ERAS) protocols-starting with early movement and eating after surgery-are cutting hospital stays by 30% and reducing readmissions. Single-incision laparoscopic surgery (SILS) is being tested, but it’s more complicated and carries higher risks than standard laparoscopy. So far, it hasn’t replaced the standard.
The biggest driver of gallstone cases? Obesity. Nearly 40% of US adults are obese. And women? They’re two to three times more likely to get gallstones than men. Hispanic populations have a 45% higher risk than non-Hispanic whites. These aren’t random. They’re tied to diet, hormones, and metabolism.
But despite new tools and better imaging, the core truth hasn’t changed: if you have symptoms, removing the gallbladder is still the safest, most effective solution. As one leading surgeon put it: ‘No matter how fancy the pills get, cholecystectomy will remain the standard for the next decade.’
What to Do If You Think You Have Gallstones
Don’t wait for the next attack. If you’ve had one episode of sudden, severe upper abdominal pain-especially after eating-get checked. An ultrasound is quick, painless, and 95% accurate at spotting stones.
If you’re diagnosed:
- Track your symptoms: How often? How bad? What triggers them?
- Ask about surgery-not just pills or waiting.
- If you’re over 75 or have other health issues, ask for a risk assessment.
- Don’t accept vague answers like ‘it might go away.’ It won’t.
- If you’re in pain now, demand proper pain relief. NSAIDs are just as effective as opioids, with fewer side effects.
Living with gallstones isn’t about managing pain. It’s about preventing disaster. And the best way to do that? Remove the source before it breaks.




Write a comment
Your email address will be restricted to us