When you pick up a generic pill from the pharmacy, you expect it to work just like the brand-name version. But behind that simple promise lies a complex, often broken system. In 2022, nearly 4,000 drug products were recalled in the U.S. alone because of manufacturing flaws. Most of these came from overseas plants where quality control is weak, inspections are scheduled in advance, and cost-cutting has replaced safety as the top priority.
Why Generic Drugs Fail: The Core Problem
Generic drugs aren’t supposed to be cheaper because they’re worse. They’re supposed to be identical in active ingredient, strength, and effect. But in practice, many fail to meet that standard. The reason? Poor manufacturing practices. The FDA calls these failures violations of Current Good Manufacturing Practices, or cGMP. These aren’t suggestions-they’re legal requirements. When a plant skips steps, uses untested raw materials, or falsifies data, the result is pills that don’t dissolve properly, contain toxic impurities, or vary wildly in potency. Take the 2018 valsartan recall. A cancer-causing impurity called NDMA showed up in blood pressure meds made in China and India. It wasn’t an accident. It was a chemical reaction caused by a change in the manufacturing process that no one tested for. Nearly 2.1 million patients were exposed. The FDA found the same problem in other ARBs, leading to 28 separate recalls over a year and a half. This wasn’t an isolated case. It was a pattern.What Goes Wrong Inside These Plants
The technical failures are specific and disturbing:- Nitrosamine impurities-carcinogens that form during chemical reactions-are now found in everything from blood pressure meds to diabetes drugs.
- Inadequate analytical methods-18.7% of FDA inspection findings relate to labs that can’t even measure what’s in the product accurately.
- Poor packaging-12.3% of issues involve moisture or light getting into pills, making them degrade before the expiration date.
- Unstable formulations-15.6% of drugs lack proper long-term stability data, meaning no one knows if they’ll work after six months on the shelf.
- Dirty facilities-FDA inspectors found employees in an Indian plant pouring acid into trash cans full of quality control documents. That wasn’t a mistake. It was destruction of evidence.
The Inspection Gap: How the System Lets Plants Slip Through
The FDA inspects U.S. plants without warning. That keeps companies honest. But for foreign plants? They get months of notice. That’s not oversight-it’s a heads-up. Plants clean up, hide problems, and even hire temporary staff just for the inspection. A 2023 Ohio State University study found generic drugs made in India caused 23.7% more severe side effects than those made in the U.S. Worse, the FDA hasn’t inspected nearly 1,000 foreign facilities that export drugs to America. That’s one-third of all foreign plants. The agency only inspects 13% of them each year, even though 73% of finished drug products come from overseas. The FDA admits it doesn’t test more than 0.02% of imported shipments. That’s like checking two random cars out of 10,000 to see if they’re safe to drive.
Who’s Getting Hurt?
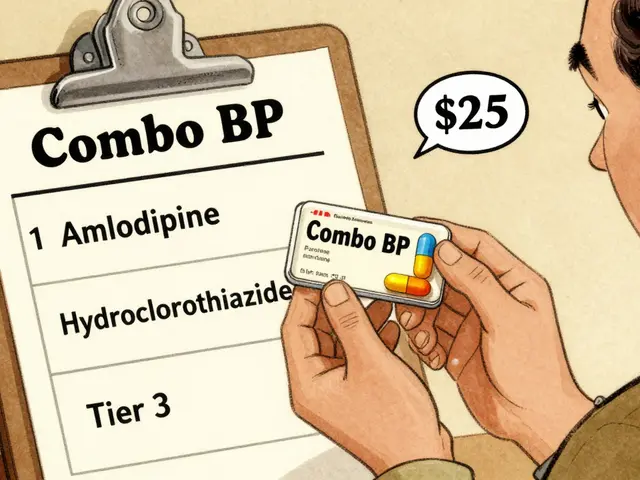
Patients are paying the price. A 2022 survey by the American Society of Health-System Pharmacists found that 67% of hospital pharmacists had seen at least one generic drug fail in the past year. Over 42% pointed to products made in India. On Drugs.com, generic valsartan from Zhejiang Huahai Pharmaceutical got a 3.2-star rating. The U.S.-made version? 4.1 stars. Reviews mention “didn’t work,” “my BP didn’t drop,” and “felt like I was getting the brand again.” The FDA’s own adverse event database shows 1,842 reports linked to quality issues between 2019 and 2022. One company, Impax Laboratories, accounted for 14.3% of those reports because their nitroglycerin tablets didn’t dissolve fast enough-dangerous for heart attack patients who need immediate relief.Why This Keeps Happening: Money vs. Safety
Generic drug prices have dropped 18.3% every year since 2018. Companies are squeezed. To stay profitable, they cut corners. Quality control budgets fell 22.7% on average. Staff training? Reduced. Lab equipment? Outdated. Data integrity? Ignored. In 2022, 78.3% of data integrity issues were due to weak passwords, no audit trails, or deleted records. Only 23.8% of generic manufacturers use Quality by Design (QbD)-a system that builds safety into the product from the start. It costs $2.7 million per facility and takes 18-24 months to implement. Most companies won’t pay it. Instead, they rely on shortcuts. The FDA’s own data shows that 31.2% of inspection findings relate to poor staff training, and 24.8% to bad recordkeeping.Who’s Responsible?
The FDA is underfunded and outgunned. The agency’s 2023 Strategic Plan admits it’s still using a 20th-century inspection model for a 21st-century global supply chain. The European Medicines Agency (EMA) changed its rules in January 2023: all foreign inspections are now unannounced. The result? A 41.2% jump in critical findings. Meanwhile, the U.S. still gives foreign plants advance notice. The White House called pharmaceutical supply chains a national security risk in 2020. Over 72% of essential medicine ingredients come from China and India. If one plant shuts down-because of a fire, a scandal, or a recall-it can trigger nationwide shortages. In 2022, 58.7% of all drug shortages were caused by quality failures at foreign plants. Medications like heparin and nitroglycerin disappeared from shelves. People died waiting.What’s Being Done-and Why It’s Not Enough
The FDA got $56.7 million in 2022 to improve foreign inspections. Their goal? Increase inspections from 1,200 to 1,800 by 2027. That sounds good-until you realize there are nearly 3,000 foreign facilities. Even with that increase, they’ll still only inspect 60% of them annually. And that’s if they get the funding. The 2023 Drug Competition Action Plan now requires 100% more stability data and 75% more bioequivalence testing for complex generics. That’s a step forward. But it’s reactive. It doesn’t stop bad plants from making bad drugs. It just makes it harder for them to get approved. The real solution? Unannounced inspections everywhere. Mandatory third-party audits. Publicly available inspection reports. Real penalties-not just warning letters that get ignored. Until then, patients are the ones taking the risk.What You Can Do
You can’t inspect a factory. But you can be aware:- If your generic drug suddenly stops working, talk to your pharmacist. Ask where it’s made.
- Check the FDA’s Drug Shortages list. If your med is on it, ask for a brand-name alternative.
- Report side effects to the FDA’s MedWatch system. One report might not change anything-but 100 could trigger an inspection.
- Support policies that fund the FDA to inspect foreign plants without warning.
Why are generic drugs more likely to have quality issues than brand-name ones?
Brand-name companies usually own their own manufacturing facilities and invest heavily in quality systems from the start. Generic manufacturers, especially overseas, often operate on thin margins and cut costs in areas like testing, training, and documentation. FDA data shows foreign generic plants receive 20-30% more inspection violations than U.S. ones. The difference isn’t the drug-it’s the factory.
How can I tell if my generic drug is from a bad manufacturer?
Look at the label. The manufacturer’s name is printed on the bottle or blister pack. Search the FDA’s website for inspection reports using that name. If you see a history of warning letters, recalls, or data integrity issues, ask your pharmacist for a different version. Some pharmacies stock multiple generic brands-ask for one made in the U.S. or the EU.
Are all drugs from India and China unsafe?
No. Many facilities in India and China meet international standards. But the problem is inconsistency. A plant might pass one inspection, then fail the next because it’s cutting corners to save money. The FDA doesn’t test every batch. So even if one lot is safe, the next might contain impurities or have poor dissolution. You can’t assume safety based on country alone.
What’s the difference between a recall and a warning letter?
A warning letter means the FDA found violations but hasn’t pulled the product yet. It’s a notice to fix things. A recall means the drug is already in your medicine cabinet and has been deemed unsafe or ineffective. Recalls happen after evidence of harm-like patients getting sick or failing to respond to treatment. Warning letters are preventable. Recalls are the consequence of ignoring them.
Why doesn’t the FDA test every shipment of imported drugs?
The FDA inspects less than 0.02% of imported drug shipments. Why? It’s impossible. The U.S. imports over 10 million shipments of drugs and ingredients each year. The agency simply doesn’t have enough labs, staff, or funding to test them all. Instead, they rely on inspections and paperwork-which manufacturers can fake. That’s why unannounced site visits are the only reliable way to catch real problems.
Can I trust my pharmacist’s advice on generic drugs?
Most pharmacists are trustworthy and want you to get safe, effective medication. But they’re not always told where a drug is made or if it’s been flagged. Ask them: “Is this made in the U.S. or the EU?” and “Has this brand had any recalls?” If they hesitate or say they don’t know, ask for a different brand. You have the right to choose.



Write a comment
Your email address will be restricted to us