More than 1 in 10 adults in the U.S. take sleep aids every night. For many, it’s the only thing that helps them fall asleep after months of tossing and turning. But what happens to your brain when you take these pills regularly? And why do some people wake up feeling foggy, forgetful, or even confused? The truth is, not all sleep aids are created equal - and some carry real risks to your thinking, memory, and long-term brain health.
What Are Sleep Aids, Really?
Sleep aids aren’t just one thing. They’re a group of very different drugs, each working in completely different ways. The most common ones include:- Benzodiazepines (like diazepam or lorazepam) - originally designed for anxiety, they’re sometimes used off-label for sleep.
- Non-benzodiazepine hypnotics (zolpidem, zaleplon, eszopiclone) - sold under brand names like Ambien, Sonata, and Lunesta.
- Antidepressants (like trazodone) - prescribed for sleep even though they’re not FDA-approved for that use.
- Melatonin receptor agonists (ramelteon) - mimic the body’s natural sleep hormone.
- Dual orexin receptor antagonists (DORAs) - newer drugs like suvorexant and daridorexant that block wakefulness signals.
Each of these has a different impact on your brain. Some slow down brain activity broadly. Others target very specific pathways. That’s why their side effects vary so much.
The Cognitive Risks: What the Science Shows
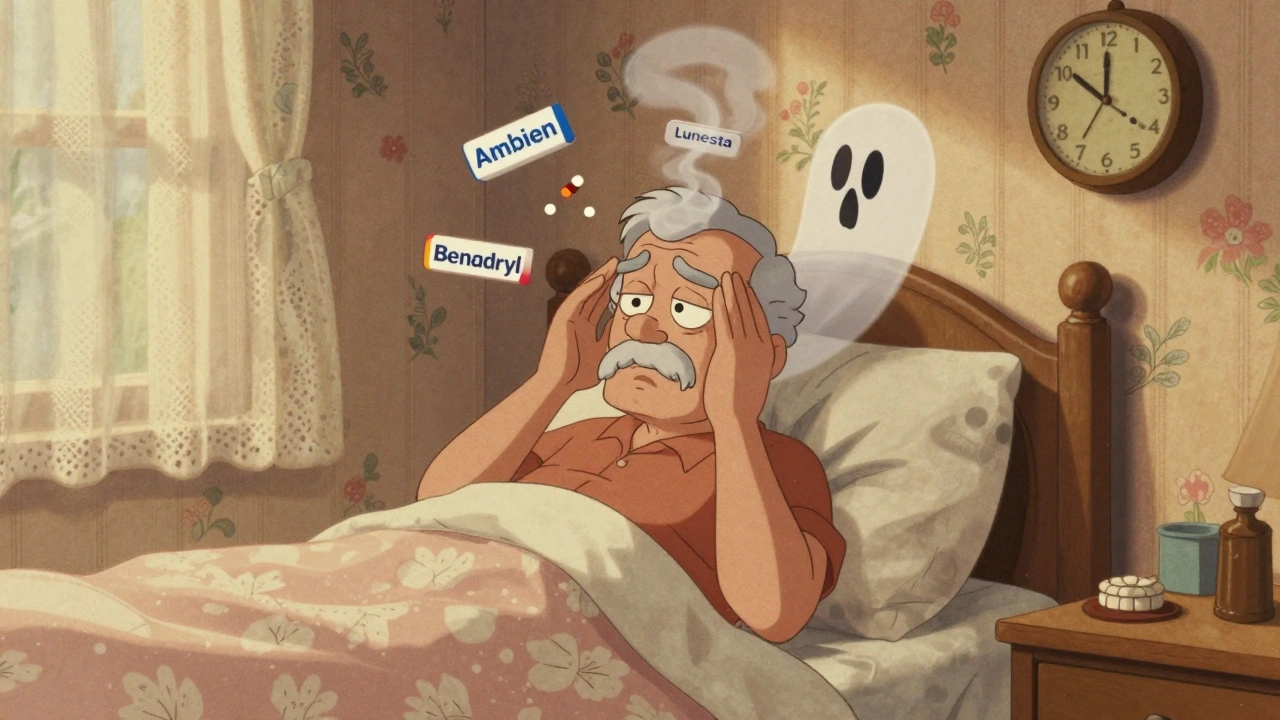
A 2021 study tracking over 3,000 older adults found that people who took sleep medications regularly had a 30% higher chance of developing dementia over the next decade. But here’s the twist: that risk wasn’t the same for everyone. White participants saw a 79% increased risk. Black participants didn’t show a significant link. Why? It might have to do with differences in metabolism, dosage, or even how often these drugs were prescribed in the first place.Then there’s the class of drugs that’s most dangerous for your brain: anticholinergics. These include some older sleep medications and even over-the-counter antihistamines like diphenhydramine (Benadryl). A landmark study from Indiana University found these drugs directly linked to mild cognitive impairment - memory loss that doesn’t yet affect daily life, but can be a warning sign. The good news? This kind of impairment might be reversible if you stop taking the drug.
On the other hand, zolpidem and trazodone - two of the most commonly prescribed sleep aids - didn’t show any clear link to memory decline in a 2019 NIH study of nearly 3,300 people. In fact, some researchers think they might even help protect the brain by improving sleep quality in people who were severely sleep-deprived.
The New Hope: DORAs and the Brain
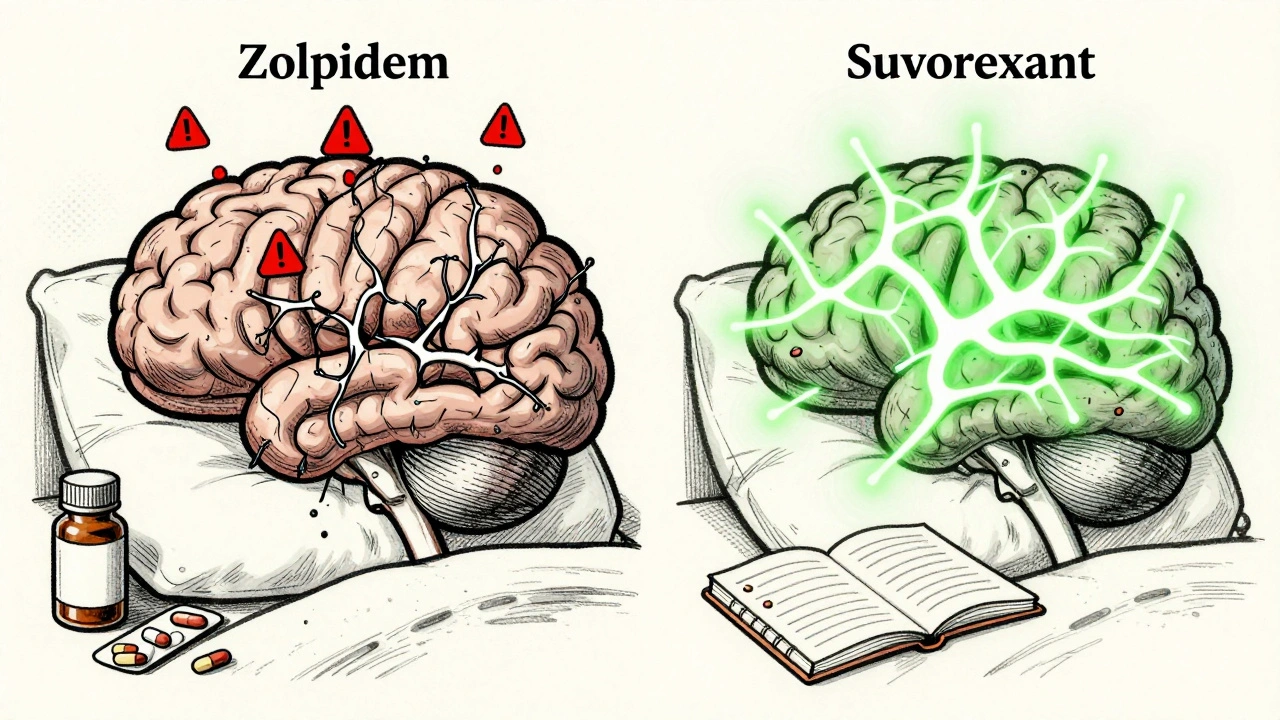
The most exciting development in sleep medicine isn’t just about helping you sleep - it’s about protecting your brain while you do.DORAs, like suvorexant (Belsomra) and daridorexant (Quviviq), work differently. Instead of calming your entire brain like benzodiazepines do, they block orexin - the brain’s wakefulness signal. Think of it like turning off a light switch instead of putting the whole house to sleep.
Here’s the remarkable part: a 2023 study at Washington University showed that people who took suvorexant for just two nights had lower levels of two proteins linked to Alzheimer’s disease - amyloid and tau. That’s never been seen before with a sleep medication. It suggests these drugs might not just help you sleep - they could be slowing down brain damage.
Animal studies back this up. When monkeys were given DORA-22 (still in testing), they slept better - but didn’t show any decline in memory or reaction time. The same monkeys given GABA-targeting drugs like zolpidem scored 20% worse on cognitive tests.
Real-world users notice the difference too. On Drugs.com, 62% of people who’ve tried suvorexant gave it 4 stars or higher, often saying they felt “clear-headed” in the morning. Compare that to zolpidem: 38% of reviews are 2 stars or lower, with users complaining about “amnesia episodes,” “brain fog,” and forgetting where they put their keys.
Who’s Most at Risk?
Age matters. Your brain changes as you get older. It becomes more sensitive to drugs that affect neurotransmitters. That’s why the American Geriatrics Society’s Beers Criteria - the gold standard for safe prescribing in older adults - says to avoid benzodiazepines, zolpidem, and tricyclic antidepressants entirely for people over 65.Why? Because these drugs increase the risk of falls, car accidents, and confusion. One study found that older adults on sleep aids were 50% more likely to have a fall that required hospitalization. And the cognitive effects? They don’t always go away after you stop taking the pill. Some people report brain fog lasting weeks or even months after quitting.
Younger people aren’t immune, but they tend to recover faster. Reddit users under 40 often report next-day grogginess with zolpidem, but rarely mention memory loss. Those over 65? They’re far more likely to describe “not remembering the night” or “waking up confused.”
What About Stopping?
If you’ve been taking sleep aids for months or years, quitting cold turkey is a bad idea. Your brain gets used to them. Suddenly stopping can cause rebound insomnia - worse than before - along with anxiety, tremors, and even seizures in extreme cases.The safest way out? Gradual tapering. Most experts recommend reducing your dose by 10-25% every week or two, under medical supervision. For benzodiazepines, that process can take 4 to 8 weeks. Don’t try to do it alone.
And here’s the kicker: the goal isn’t just to stop the drug. It’s to replace it with something better.

The Real Solution: CBT-I
The American College of Physicians says it clearly: cognitive behavioral therapy for insomnia (CBT-I) should be the first treatment for chronic insomnia - not pills.CBT-I isn’t about counting sheep. It’s a structured program that teaches you how to fix the thoughts and habits keeping you awake. It includes sleep scheduling, stimulus control (like only using your bed for sleep), and cognitive restructuring (challenging beliefs like “I need 8 hours or I’ll die”).
Studies show CBT-I works better than any sleep aid in the long run. People who complete it stay asleep longer, wake up less, and report better mood and focus - without a single pill. And the effects last. Five years later, most people still sleep well.
But it’s not easy. You need 6 to 8 weekly sessions with a trained therapist. Each one is about 50 minutes. The cost? Up to $1,500 if done in person. But digital options like Sleepio and CBT-I for Insomnia have proven just as effective, for $300-$500. The American Academy of Sleep Medicine lists over 1,200 certified CBT-I providers across the U.S. as of early 2024.
The Bigger Picture
The sleep aid market was worth $85.7 billion in 2023. But sales of traditional pills are slowing. Meanwhile, non-drug solutions are growing at nearly twice the rate. Why? Because people are waking up - literally and figuratively - to the cost of sleeping pills.The FDA added stronger warnings to benzodiazepine labels in late 2022. Pharmaceutical companies are pouring money into next-gen DORAs. The National Institutes of Health just launched a 15-year study tracking 10,000 people to see how sleep meds affect brain aging. And the Alzheimer’s Association now lists poor sleep as one of the top modifiable risk factors for dementia.
This isn’t just about getting a good night’s rest. It’s about protecting the most important organ you have - your brain.
What Should You Do?
If you’re on a sleep aid right now, here’s what to ask yourself:- How long have I been taking this? (More than 3 months? Time to plan an exit.)
- Do I feel groggy or foggy in the morning? (That’s a red flag.)
- Have I noticed memory lapses? (Even small ones matter.)
- Am I taking it because I’m scared I won’t sleep without it? (That’s dependency, not treatment.)
Don’t panic. Don’t quit cold turkey. But do talk to your doctor. Ask about CBT-I. Ask if there’s a safer alternative. Ask about your long-term brain health - not just tonight’s sleep.
Because the best sleep aid isn’t a pill. It’s a well-rested brain that doesn’t need help to shut down - and doesn’t pay for it the next day.
Can sleep aids cause dementia?
Some sleep aids, especially long-term use of benzodiazepines and anticholinergic drugs, are linked to a higher risk of dementia. But not all sleep medications carry the same risk. Newer drugs like suvorexant (a DORA) may even reduce Alzheimer’s-related brain proteins. The key is the type of drug, how long you take it, and your age. Always talk to your doctor about your specific risk.
Do all sleep aids make you feel foggy in the morning?
No. Older drugs like zolpidem and benzodiazepines often cause next-day grogginess, memory issues, and brain fog. But newer DORAs like suvorexant and daridorexant are designed to leave your brain clear in the morning. User reviews and clinical studies show significantly less morning impairment with these newer options.
Is trazodone safe for long-term sleep use?
Trazodone isn’t FDA-approved for sleep, but it’s commonly prescribed off-label. Studies show it doesn’t increase dementia risk like benzodiazepines do. However, it can cause dizziness, dry mouth, and low blood pressure - especially in older adults. While safer than some options, it’s still not ideal for long-term use. CBT-I is a better choice for lasting results without side effects.
Can I stop taking sleep aids cold turkey?
No. Stopping suddenly - especially after using benzodiazepines or zolpidem for weeks or months - can cause rebound insomnia, anxiety, tremors, or even seizures. Always work with your doctor to taper off slowly, usually over 4-8 weeks. Never quit on your own.
What’s the best non-drug alternative to sleep aids?
Cognitive Behavioral Therapy for Insomnia (CBT-I) is the most effective, evidence-based alternative. It teaches you how to change thoughts and habits that keep you awake. Studies show it works better than medication long-term, with no side effects. Digital programs like Sleepio offer the same results for a fraction of the cost of in-person therapy.





Write a comment
Your email address will be restricted to us