If you’ve been prescribed Benemid (probenecid) for gout or high uric acid levels, you’re probably wondering if there are better or simpler options. Maybe you’re dealing with side effects, or the cost is rising, or your doctor mentioned another drug. You’re not alone. Many people on probenecid ask the same thing: Are there alternatives that work just as well-or better?
What Benemid (Probenecid) Actually Does
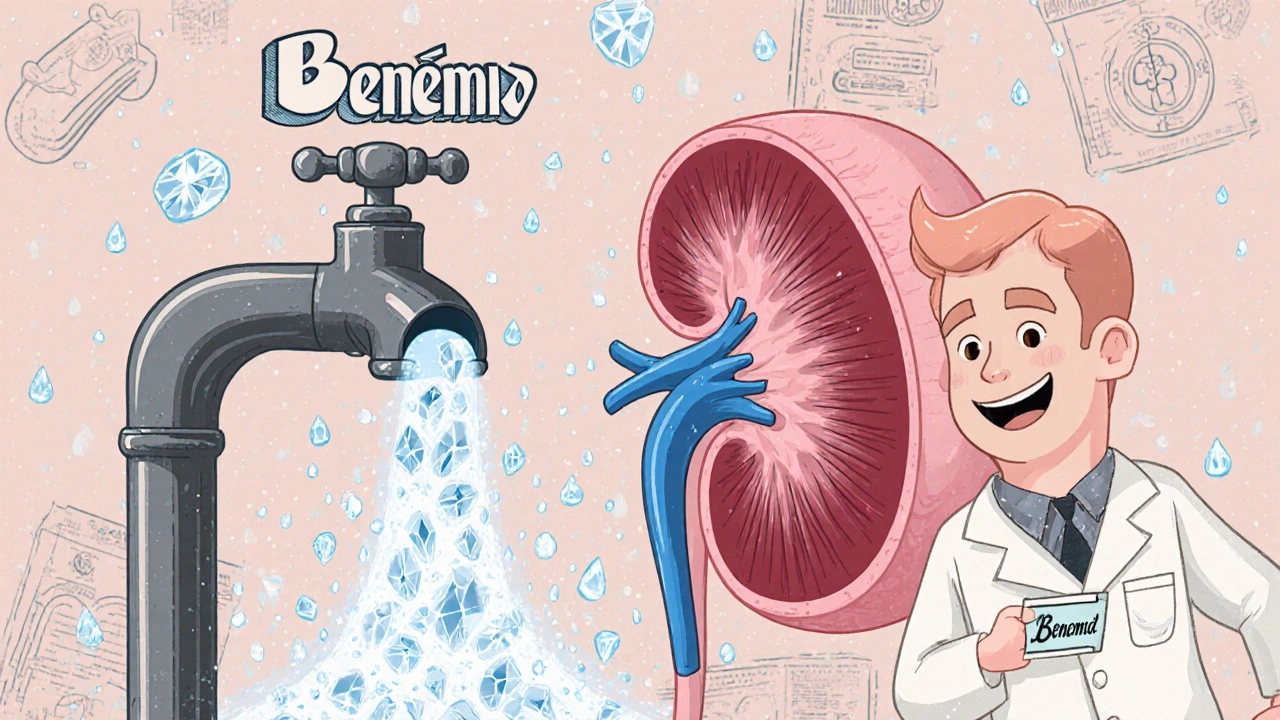
Benemid is the brand name for probenecid, a medicine that’s been around since the 1950s. It doesn’t reduce how much uric acid your body makes. Instead, it tells your kidneys to flush more of it out through urine. That lowers the level of uric acid in your blood, which helps prevent gout attacks and kidney stones caused by uric acid crystals.
It’s not a painkiller. You won’t feel relief during a flare-up. Benemid is for long-term control. People usually take it daily, often with plenty of water to avoid kidney stones. Typical doses range from 500 mg to 2,000 mg per day, split into two doses.
But here’s the catch: probenecid only works if your kidneys are still doing a decent job. If you have advanced kidney disease, it’s not going to help much. And it can cause side effects like stomach upset, rashes, or even kidney stones if you don’t drink enough fluids.
Allopurinol: The Most Common Alternative
Allopurinol is the most widely prescribed alternative to Benemid. While probenecid helps your body get rid of uric acid, allopurinol stops your body from making too much of it in the first place. It targets the enzyme xanthine oxidase, which is responsible for producing uric acid.
Studies show allopurinol reduces serum uric acid levels more consistently than probenecid, especially in people who overproduce uric acid-about 80% of gout patients. It’s also cheaper, available as a generic, and taken once a day. Most people start at 100 mg and increase slowly to avoid flare-ups.
But allopurinol isn’t perfect. About 2% of people have a severe allergic reaction called allopurinol hypersensitivity syndrome, which can be life-threatening. People of Asian descent, especially those with the HLA-B*58:01 gene, are at higher risk. Some doctors now test for this gene before prescribing allopurinol.
Febuxostat: For When Allopurinol Doesn’t Work
If you can’t take allopurinol due to allergies or side effects, febuxostat is the next go-to. Like allopurinol, it blocks uric acid production. But it works differently-it’s not a purine analog, so it’s less likely to cause reactions in people allergic to allopurinol.
Febuxostat is usually taken as a 40 mg or 80 mg tablet once daily. It’s more effective at lowering uric acid than allopurinol at standard doses, especially in patients with moderate kidney impairment. A 2020 study in The New England Journal of Medicine found that 55% of patients on 80 mg of febuxostat reached target uric acid levels under 6 mg/dL, compared to 45% on allopurinol.
But febuxostat has its own risks. The FDA added a black box warning in 2019 after a trial showed a higher risk of heart-related death compared to allopurinol. If you have heart disease or stroke history, your doctor will likely avoid febuxostat.
Lesinurad: Used Only With Another Drug
Lesinurad (Zurampic) is a newer option that works like probenecid-it helps your kidneys remove uric acid. But it’s not used alone. It’s always combined with either allopurinol or febuxostat. It’s designed for people who haven’t reached their uric acid goal with a single drug.
Studies show adding lesinurad to allopurinol can push uric acid levels below 5 mg/dL in up to 60% of patients who didn’t respond to allopurinol alone. But it’s expensive and carries a risk of kidney injury. You must take it with food and drink at least 2 liters of water daily. Many doctors avoid it unless other options have failed.
Colchicine: Not a Replacement, But a Helper
Colchicine is often confused with uric acid-lowering drugs. It’s not. It doesn’t reduce uric acid at all. Instead, it reduces inflammation during gout flares. Many people take low-dose colchicine (0.6 mg once or twice daily) long-term to prevent flares while their uric acid reducer-like allopurinol or probenecid-takes effect.
It’s especially useful in the first 6 months of starting a uric acid-lowering drug, when flares can spike as crystals dissolve. Colchicine is cheap, well-tolerated at low doses, and has been used for centuries. But high doses cause severe diarrhea, nausea, and muscle weakness.
What About Natural Options?
People often ask about cherry juice, baking soda, or vitamin C as alternatives. There’s weak evidence that cherry extract might slightly reduce flare frequency. Vitamin C in high doses (500 mg daily) may lower uric acid by about 0.5 mg/dL on average. But these aren’t replacements for prescription meds.
If you’re trying to avoid medication, lifestyle changes matter more than supplements. Losing 10% of your body weight can cut uric acid levels by 1-2 mg/dL. Cutting out sugary drinks, especially fructose-sweetened sodas, has a bigger impact than most pills. Alcohol-especially beer and spirits-raises uric acid sharply. One study found that men who drank two beers a day had a 90% higher risk of gout.
Choosing the Right Option for You
There’s no single best drug. The right choice depends on your body, your health history, and your goals.
- If your kidneys are healthy and you overexcrete uric acid, probenecid might still be fine.
- If you overproduce uric acid (most common), allopurinol is usually first-line.
- If you’re allergic to allopurinol or can’t tolerate it, febuxostat is the next step.
- If you’re not reaching target levels on one drug, adding lesinurad could help-but it’s expensive and risky.
- If you’re having frequent flares, colchicine can help until your main drug kicks in.
Your doctor will check your kidney function, liver enzymes, and possibly your genetic profile before deciding. They’ll also look at your uric acid level goals-usually under 6 mg/dL, and under 5 mg/dL if you have tophi (uric acid lumps under the skin).
Why Some People Switch from Benemid
People stop taking probenecid for a few common reasons:
- They need to take it twice a day and forget doses.
- They get stomach pain or diarrhea.
- They develop kidney stones despite drinking lots of water.
- They find out their kidneys aren’t working well enough for it to help.
- They’re on other medications that interact with probenecid, like aspirin or certain antibiotics.
Switching to allopurinol or febuxostat often solves these problems. One 2023 survey of 1,200 gout patients in the UK found that 68% of those who switched from probenecid to allopurinol reported fewer flares and better adherence within six months.
What Happens If You Stop Without a Plan?
Stopping any uric acid-lowering drug suddenly can trigger a gout flare. Your body has adjusted to lower uric acid levels. When you stop, crystals can suddenly dissolve and trigger inflammation.
If you’re thinking of quitting Benemid, talk to your doctor first. They may recommend tapering slowly or starting another medication before stopping. Never stop cold turkey.
Cost and Accessibility
Benemid (probenecid) is available as a generic, so it’s usually cheap-around £10-£15 per month in the UK. Allopurinol is even cheaper, often under £5. Febuxostat is more expensive, around £40-£60 monthly, and may require prior authorization from your health provider. Lesinurad is the most expensive, often over £100, and rarely stocked in community pharmacies.
Insurance coverage varies. In the NHS, allopurinol is first-choice for most patients. Febuxostat is usually only approved if allopurinol isn’t suitable. Probenecid is rarely prescribed now unless there’s a specific reason.
Bottom Line: What Should You Do?
Benemid (probenecid) is a valid option, but it’s not the first choice anymore for most people. Allopurinol is simpler, cheaper, and more effective for the majority. Febuxostat is a strong alternative if you can’t take allopurinol. Lesinurad has a narrow use case. Colchicine helps with flares but doesn’t lower uric acid.
If you’re on Benemid and doing well-no side effects, no flares, your uric acid is under control-there’s no need to switch. But if you’re struggling with side effects, forgetting doses, or your doctor says your kidneys aren’t responding, ask about switching to allopurinol. It’s the most proven, safest, and most affordable long-term solution for most people.
And remember: medication alone won’t fix gout. Diet, weight, and hydration matter just as much. One patient in Manchester I spoke with reduced his flares from 4 a year to zero after cutting out sugary drinks, losing 15 pounds, and taking allopurinol. He didn’t need Benemid at all.
Is Benemid still commonly prescribed for gout?
Not usually. Allopurinol is the first-line treatment in the UK and most of the world. Benemid (probenecid) is now mostly used when allopurinol or febuxostat can’t be taken, or in rare cases where the patient overexcretes uric acid and has healthy kidneys. It’s considered a second- or third-line option today.
Can I take probenecid and allopurinol together?
Yes, but it’s rare. Combining them is sometimes done if uric acid levels remain high despite maximum doses of one drug. However, most doctors prefer to increase allopurinol first, since it’s more effective at lowering uric acid overall. Combining drugs increases side effect risks and cost, so it’s only done when absolutely necessary.
Does probenecid cause kidney damage?
Not directly, but it can contribute to kidney stones if you don’t drink enough water. Probenecid increases uric acid excretion, which can lead to crystal buildup in the urinary tract. It’s also not recommended if you already have severe kidney disease (eGFR below 30), because it won’t work well and may worsen the condition. Regular kidney function tests are required while taking it.
How long does it take for probenecid to work?
It doesn’t work quickly. You won’t feel better during a gout attack. It can take 2-6 weeks for uric acid levels to drop enough to prevent new attacks. Some people still get flares in the first few months as crystals dissolve. That’s why doctors often prescribe colchicine at the start to prevent flares.
What’s the most effective drug for lowering uric acid?
For most people, allopurinol is the most effective and safest long-term option. Febuxostat works better in some cases, especially with kidney issues, but carries a higher heart risk. Lesinurad boosts uric acid reduction when added to another drug but isn’t used alone. Probenecid is less effective overall and requires strict hydration. The best drug depends on your body, not a one-size-fits-all answer.



Write a comment
Your email address will be restricted to us