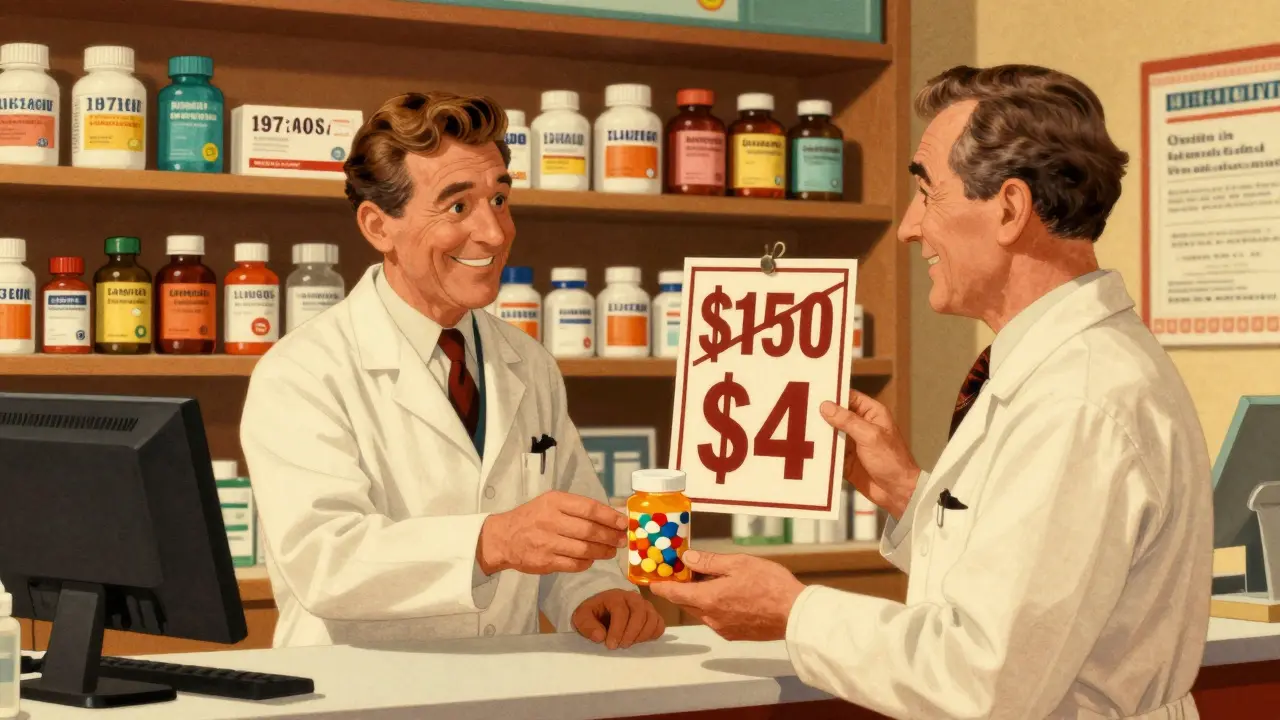
Switching to generic medications isn’t just a smart move-it’s one of the easiest ways to cut your monthly drug costs by 85% without changing how your treatment works. If you’re paying $150 for a brand-name pill, there’s a very good chance you could get the exact same medicine for under $5. And no, it’s not a trick. The FDA requires generics to work identically in your body. The active ingredient? Same. The dose? Same. The way it’s absorbed? Same. The only real difference? The price tag.
Why Generics Cost So Much Less
Brand-name drugs aren’t cheaper because they’re better. They’re expensive because the company that invented them spent years and millions developing it, running clinical trials, and marketing it. Once the patent runs out-usually after 10 to 12 years-other companies can make the same drug. They don’t need to repeat those expensive trials. They just have to prove their version delivers the same amount of medicine into your bloodstream at the same speed. That’s it. No extra testing. No new research. Just manufacturing.The result? A 90% drop in price. Take a common blood pressure pill: brand-name version might cost $1,400 for a 30-day supply. The generic? Under $60. That’s not a guess. That’s FDA data from 2022. Another drug went from $88 per milliliter to under $10. That’s a 90% drop. Across the U.S., these savings added up to over $2.2 trillion in the last decade. That’s not a rounding error. That’s real money back in people’s pockets.
Are Generics Really the Same?
Yes. And the FDA doesn’t let them get away with anything less.Every generic drug must meet the same strict standards as the brand-name version: same strength, same purity, same stability. The same factories that make brand-name drugs often make generics too-just under a different label. The FDA inspects both types of facilities the same way. If a generic fails to meet the standard, it’s pulled off the market.
The only differences you’ll notice? The color, shape, or taste. Maybe the pill has a different logo or a different filler ingredient. Those don’t affect how the medicine works. They’re just there to make the pill look different and avoid trademark issues. You might even see a generic labeled with the chemical name-like “metformin” instead of “Glucophage.” That’s normal.
Some people say, “I feel different on the generic.” That’s usually not the medicine changing. It’s your brain noticing the pill looks different. Or maybe you switched from a brand that used one filler to a generic that used another, and you’re sensitive to that. Rarely, with drugs that have a very narrow therapeutic window-like levothyroxine for thyroid issues-do doctors recommend sticking with one brand. But even then, switching between generics is usually fine. Talk to your pharmacist if you’re unsure.
How Much Can You Actually Save?
Let’s get specific. Here’s what real people are saving in 2026:- One man in Phoenix saves $300 a month on his daughter’s medications by switching to generics-hundreds a year, just from one prescription.
- A Reddit user switched from a $150 brand-name antidepressant to a $4 generic. Same effect. Same side effects. Zero extra cost.
- Medicare Part D beneficiaries can buy 90% of the most common generic drugs at Costco for under $20 for a 30-day supply.
- Uninsured patients using the Mark Cuban Cost Plus Drug Company (MCCPDC) save an average of $6 per prescription-some over $10. That’s not a discount. That’s a reset of the whole pricing system.
Even if you have insurance, generics often cost less than your copay. Some plans charge $10 for a generic but $50 for the brand-name version-even if the generic is cheaper than the copay. Your pharmacy can often switch you automatically, but you have to ask. Don’t assume they’re doing it.

How to Start Using Generics
It’s easier than you think. Here’s how to get started:- Check your prescription. Look at the name. If it’s a brand name like “Lipitor” or “Prozac,” ask your doctor or pharmacist if there’s a generic. Most are.
- Ask your pharmacist to substitute. In most states, pharmacists are allowed to swap in a generic unless the doctor says “dispense as written.” Even if they don’t do it automatically, just ask.
- Compare prices at different pharmacies. Costco, Walmart, and CVS often have generics for under $10-even if you don’t have insurance. Some are $4 for a 30-day supply.
- Try the Mark Cuban Cost Plus Drug Company (MCCPDC). It’s a direct-to-consumer pharmacy with transparent pricing. No insurance needed. You pay the cost of the drug plus a $5 fee. No markups. No middlemen.
- Use your pharmacy’s discount program. Many have loyalty cards or apps that drop generic prices even lower.
You don’t need to change doctors. You don’t need to jump through hoops. Just ask. And if your pharmacist says “no,” ask why. Sometimes, it’s just inertia.
What About Complex Drugs? Biologics and Biosimilars
Not all drugs have generics. Biologics-like insulin, rheumatoid arthritis drugs, or cancer treatments-are made from living cells, not chemicals. They’re harder to copy. But that’s changing.Biosimilars are the next wave. They’re not exact copies, but they’re close enough to be approved as safe and effective. The FDA has approved dozens already. And they’re cheaper. Much cheaper. One insulin biosimilar cut the price from $300 to $50 per vial. That’s life-changing for people who need it every day.
Don’t assume your complex drug has no affordable option. Ask your doctor or pharmacist if a biosimilar exists. They’re becoming more common every year.
Why Some People Still Resist
You’ll hear stories: “My cousin switched and it didn’t work.” “I felt weird on the generic.”Here’s the truth: In most cases, it’s not the drug. It’s the change. People notice the pill looks different. They start worrying. That worry can make them feel worse-even if the medicine is doing exactly what it should.
Also, some patients are used to paying more and assume more expensive = better. That’s not how medicine works. A $150 pill isn’t more powerful than a $5 one if they’re chemically identical.
And yes, there are rare cases where switching between generics causes issues-mostly with drugs that need very precise blood levels. But those are exceptions. Your doctor or pharmacist will flag them.

What’s Next for Generic Medications?
The FDA is approving more generics than ever. In 2022 alone, hundreds of new ones hit the market. More competition means lower prices. More people are using them-90% of all prescriptions in the U.S. are generics now. That’s up from 78% in 2010.Companies like MCCPDC are challenging the old pharmacy benefit manager system. They’re proving you don’t need insurance to get affordable meds. And as more blockbuster drugs lose patents-like Humira, Ozempic, and others-the flood of generics will only grow.
The future? More biosimilars. More transparency. More savings. And more people finally able to afford the medicines they need.
Final Thought: Don’t Pay More Than You Have To
Medications aren’t luxury items. They’re necessities. If you’re paying $100 a month for a pill that has a $5 generic version, you’re overpaying. Not because you’re being careless. Because the system is broken.Switching to generics doesn’t mean you’re settling. It means you’re smart. You’re using the system the way it was designed-to save lives and money. And if you’re not asking about generics, you’re leaving money on the table. Every month.
Start today. Check your next prescription. Ask one question: “Is there a generic?”
Are generic medications as effective as brand-name drugs?
Yes. The FDA requires generic drugs to contain the same active ingredient, in the same strength, and deliver it to your bloodstream at the same rate as the brand-name version. They must meet the same quality, safety, and effectiveness standards. Thousands of studies and real-world use confirm they work the same way.
Why do generic pills look different from brand-name ones?
By law, generic drugs can’t look exactly like the brand-name version to avoid trademark infringement. That’s why the color, shape, or markings are different. But those changes are only cosmetic. They don’t affect how the medicine works. The active ingredient is identical.
Can I switch from a brand-name drug to a generic without talking to my doctor?
In most cases, yes. Pharmacists are allowed to substitute generics unless your doctor wrote “dispense as written” on the prescription. Even if they don’t do it automatically, you can ask. Your doctor doesn’t need to be involved unless you’re on a narrow therapeutic index drug like levothyroxine or warfarin-where small changes matter. Even then, switching between generics is usually safe.
Do generics cost less because they’re lower quality?
No. Generic manufacturers must meet the same FDA standards as brand-name companies. Their factories are inspected the same way. The only difference is cost structure. Generics skip the expensive research and marketing phase, which is why they’re cheaper-not because they’re made with inferior materials.
What if my insurance won’t cover the generic?
That’s rare, but it can happen. Sometimes insurance plans have formularies that favor brand-name drugs for unclear reasons. Ask your pharmacist to check if the generic is on the formulary. If not, request a prior authorization. Often, the insurance will approve it after a quick review. If you’re uninsured, pay cash at Walmart, Costco, or MCCPDC-you’ll likely pay less than your insurance copay.
Are there any drugs that don’t have generics?
Most common medications do. But newer drugs, especially biologics like insulin, Humira, or Enbrel, are harder to copy. For these, biosimilars are the alternative-similar, not identical, but proven safe and effective. Biosimilars are growing fast and are often 15-35% cheaper than the brand-name version. Ask your pharmacist if a biosimilar is available.
Can I trust generics from other countries?
Only if they’re sold by U.S.-licensed pharmacies. The FDA doesn’t regulate drugs imported from other countries. Buying from international online pharmacies can be risky-you might get counterfeit, expired, or contaminated medicine. Stick to U.S. pharmacies, even if you’re paying cash. The savings are still huge, and you’re protected by U.S. safety standards.
Next Steps: Start Saving Today
Take your next prescription to the pharmacy. Ask: “Is there a generic?” If they say no, ask why. If they say yes, ask: “How much will it cost without insurance?” Then compare that to your copay. You might be surprised. Most people find they can save $20-$100 per month-easily $200-$1,200 a year-just by switching. That’s a vacation. A car repair. A month’s groceries. All from one simple question.Don’t wait for your next refill. Do it now. Your wallet-and your health-will thank you.








Write a comment
Your email address will be restricted to us